Healthcare Reimbursement Trends in 2026: How AI Is Transforming the Reimbursement Process
Improving patient participation and empowering them to take control of their healthcare journey can enhance clinical outcomes, boost financial stability, and cut revenue losses. Healthcare businesses may increase patient involvement, decrease complications, cut down on unnecessary visits, and lower emergency admissions. This results in increased reimbursements while improving patient experience by learning more about patient behavior.

Solve Rising Claim Denials & Slow Payments with Smart Technology Built to Streamline Healthcare Reimbursement

“The successful alliance of AI and healthcare has morphed into improved patient healthcare in areas ranging from hospital productivity and patient safety to quality medical treatment. AI as a tool and/or technology is used to analyze and visualize patient data for adequate healthcare administration. Much of the research on the influence of AI on medical outcomes has been beneficial and encouraging.”– National Library of Medicine
How Quality Improvement is Redefining Healthcare Reimbursement Trends
Paying for medical services and raising quality go hand in hand. For example, value-based care payment systems make it clear that a doctor’s remuneration is determined by the quality of care they give. They are encouraged to focus on their patients’ results through this healthcare reimbursement model. On the other hand, fee-for-service could unintentionally lead to the use of extra services without necessarily enhancing patient care.
The Impact of Healthcare Reimbursement Model on Quality Care
- Paying physicians and nurses according to their value increases the likelihood that they will enhance patient outcomes. This suggests that general service quality might significantly improve.
- When healthcare professionals receive fair compensation, they may invest in quality enhancement projects, including staff training, process optimization, and technological advancements.
- Physicians must treat patients more fully and consider their immediate and long-term health when paid based on how well they do.
How Does Healthcare Reimbursement Work?
Healthcare providers must comprehend how reimbursement operates because there are numerous healthcare reimbursement model schemes accessible, each of which operates differently. Three essential elements in the process, claims submission, payer adjudication, and provider payment, ensure accurate compensation.
The first stage is for medical providers to submit comprehensive records of the services they have provided to payers or insurance companies. Comprehensive patient information, treatment details, diagnosis codes, and related expenses are all included in the application. For prompt processing and the avoidance of denials, these claims must be accurate and comprehensive.
The insurance company then evaluates and verifies the filed claims for authenticity, accuracy, and compliance with policies and regulations. This allows the insurance company to use the reimbursement method to calculate the amount to be reimbursed to the provider.
Finally, the supplier gets paid for the services provided if the claim is accepted. However, negotiated prices, co-pays, deductibles, and other elements in the provider’s contract with the payer may cause the final finances to differ.
Check Our Case Study: From Months to Minutes: AI-Driven Ingredient Intelligence Revolutionizing OTC Drug Discovery
Embracing Technology for Enhanced Billing Accuracy
Adopting technology is essential for preserving accuracy and efficiency as healthcare billing gets more complicated. To reduce errors that can result in claim denials and reimbursement delays, sophisticated billing software and automation solutions are essential. Before claims are filed, for example, combining AI and machine learning can aid in the processing of enormous volumes of data to find typical billing problems. This proactive strategy minimizes the need for expensive and time-consuming resubmissions by ensuring that claims are correct the first time.
Additionally, complex algorithms are used by provider operations software development services to expedite the handling and processing of claims. These technologies increase the accuracy and speed of billing processes by automating repetitive tasks, freeing employees to concentrate on more intricate parts of the process.
Key Challenges Businesses Are Facing in Healthcare Reimbursement
Healthcare organizations can create efficient plans to address reimbursement issues by determining the reasons behind delays and non-payments. Here’s a closer look at the reasons why healthcare reimbursement problems frequently arise:
- Rising Claim Denials: Reimbursements are either delayed or lost because of claim denials, costing hospitals millions of dollars in lost income. 38% of healthcare providers report that at least 10% of their claims are rejected. Reimbursement times are getting longer, according to 67% of respondents. The average health system saw a 56% rise in Medicare Advantage Plan payment denials. Despite a 90% increase in maintenance expenditure and a 35% increase in other operational costs, these denials resulted in a 28% drop in cash reserves.
- Complex Prior Authorization Process: Healthcare organizations may unintentionally encounter problems with healthcare reimbursement trends when they neglect to acquire prior authorization when it is required. Payers utilize prior authorization as a cost-control measure to verify the rationale for expensive medical services. The administrative burden of prior authorization is significant and time-consuming. On average, each healthcare provider completes 43 prior authorizations every week, which takes 12 hours to complete. Even worse, over 25% of physicians claim that prior authorizations are frequently or consistently rejected.
- Staffing Shortages & Lack of Appropriate Training: Healthcare organizations may experience payment problems because of workforce shortages and underqualified personnel handling revenue cycle management procedures. 70% of those surveyed said that payer reimbursement is being severely hampered by staff shortages, and 83% said that it is getting harder to follow up on overdue payments or help patients who are struggling financially.
Why Value-Based Care Matters
Most stakeholders in the healthcare system, including patients, healthcare providers, health plans, and governmental organizations, want to improve patient health outcomes in relation to the cost of care. Value-based care initiatives can connect care coordination with pleasant patient experiences by focusing on the patient care outcomes that are most important to patients. Value-based care models emphasize improving health outcomes and bringing patients and physicians together. Physicians spend less time on paperwork and more time on wellness when value-based reimbursement functions as planned.
Improved results lower the requirement for continuing treatment and cut costs. Value-based payment models can assist in lowering the likelihood of illness progression, which increases the need for additional care, by improving health outcomes. For instance, fewer diabetics will eventually develop renal failure or neuropathy because of the value-based reimbursement that CMS (Centers for Medicare & Medicaid Services) is working toward.
Value-based healthcare, also known as CMS pay for performance or value-based care CMS, focuses on improving the health of many people. To provide efficient and appropriate value-based care, the CMS value-based care model places decision-making authority in the hands of the clinical team and primary care physician.
VBR’s primary goal is to provide a healthcare setting that:
- Promotes preventive healthcare.
- Encourages the coordination of care between various providers.
- Decreases readmissions to hospitals and needless procedures.
- Synchronizes patient outcomes with provider performance.
Check Our Case Study: Technical Accelerator Diligence: Future-Proofing a Digital Health Platform
Why Modern Healthcare Reimbursement Technology is No Longer Optional
An outdated payment system is not only an annoyance but also a major vulnerability in today’s complex healthcare setting, characterized by rising operating expenses, declining margins, and increasing patient financial responsibility. Adopting modern healthcare payment technologies is now essential to both patient satisfaction and financial stability. Every stakeholder in the ecosystem benefits from it.
For Providers
Modern payment technology has clear and quantifiable benefits for hospitals, clinics, and private practices, affecting everything from daily cash flow to long-term strategic planning.
- Faster Cash Flow and Shorter A/R Cycles: The speed of payment is by far the biggest advantage. Providers can collect patient-responsible balances more quickly by providing easy digital choices like text-to-pay and online portals. The “Days in Accounts Receivable” (A/R), a crucial indicator of a provider’s financial health, is significantly decreased when claims submission and reconciliation are automated.
- Better Data Integrity, Fewer Claim Denials: One of the main causes of claim denials is manual data entry. These mistakes are eliminated by integrated systems that import patient data straight from the EHR into the billing platform. This “clean claims” strategy results in quicker, more consistent revenue, fewer rejections, and less time spent on appeals.
For Patients
Historically, the most problematic aspect of a patient’s healthcare experience has been their financial journey. By emulating the smooth experiences they have in other industries, modern technology in a healthcare payment system resolves this issue.
- Unmatched Transparency in Care Costs: Financial uncertainty is the main cause of patient stress. To give patients a trustworthy, upfront estimate of their out-of-pocket expenses, modern systems can be integrated with eligibility and estimate of tools. This openness fosters great trust by enabling patients to make educated choices and budgets for their care.
- More Effective Communication for Better Engagement: These systems serve as communication centers and processing payments. A better and less stressful financial experience is facilitated via secure chat within a portal, automated reminders for impending obligations, and confirmations of payments received. Patient satisfaction is increased overall, and confusion is decreased because of this proactive communication.
Reduce Administrative Burden and Coding Errors Through Intelligent Automation Designed for Modern Healthcare Reimbursement Needs
Emerging Healthcare Reimbursement Trends Shaping the Future
Medical billing and the entire revenue cycle can be accelerated by processing claims in healthcare reimbursement trends. Healthcare providers can benefit from healthcare insurance and reimbursement thanks to these five technologies.
 1. The Rise of Paperless & Automated Billing Workflows
1. The Rise of Paperless & Automated Billing Workflows
Paper bills will soon become obsolete. Only 9% of consumers prefer to pay their medical bills by paper check, even though over 70% of consumers receive their bills via mail, according to a recent poll on healthcare payment methods. 91% of them want electronic payment options. Compared to sending multiple bills before getting paid, sending patient bills electronically saves time and money.
Paperless billing is used and accepted in many industries. Even though eStatements are a billing alternative offered by many medical practices, adoption still has to be increased. You can avoid sending patients a bill by encouraging them to sign up for eStatements through text or email, even prior to appointments.
2. Revenue Cycle Management Becomes a Strategic Priority
Periodically optimizing the revenue cycle helps ensure that money is available when needed. Offering a variety of payment options and using electronic registration and payment systems are now popular ways to maximize the revenue cycle. These can reduce the AR cycle and produce income based on the point of service.
The speed at which healthcare organizations can access their funds is another important consideration. In addition to offering real-time visibility into financial positions, funds received by an organization on the same day or the next business day can be managed more efficiently. To improve staff productivity and cash flow, healthcare administrators should consider revenue cycle management healthcare software.
3. Growing Adoption of Contactless Registration and Payments
Customers nowadays want to feel independent. The only way to give them that feeling is through digital tools, and this also applies to healthcare payments. The opinions of consumers and providers regarding digital possibilities, however, differ greatly. 40% of clinicians believe that billing and collection have little bearing on the patient’s experience, according to this survey. Conversely, 49% of customers stated that they would favor a supplier who can offer a smooth payment process.
This situation can be significantly improved with the use of digital health instruments. Encouraging providers to use online channels for registration and payment can improve patient satisfaction and draw in additional business. In addition to being cognizant of the inherent complexity of the payments and healthcare industries, providers must select an IT vendor with a proven track record of implementing innovative payment technology.
4. Data-Driven Decision-Making in Reimbursement Models
Healthcare businesses are realizing the potential of data to make more intelligent payment decisions as data analytics tools progress. Finance teams can find trends that improve their cash flow and help them anticipate payment requirements more precisely by examining payment patterns, invoice histories, and vendor performance.
To make better judgments about payments and budgeting in 2026, healthcare finance teams must go beyond basic reporting and implement predictive analytics. With the correct data, teams may find inefficiencies in the AP system, predict when payments will be made, and even bargain with vendors for better terms based on past payment performance. Healthcare firms can cut expenses and prevent payment delays while maintaining the viability of their operations by incorporating these data-driven insights into their accounts payable strategies.
5. The Expansion of Electronic and Digital Payment Ecosystems
Healthcare teams typically make higher monthly payments than businesses in other industries, as we discussed above. More monthly queries from vendors are frequently a result of this large volume of bills. Unfortunately, 46% of healthcare AP teams waste more than six hours a month answering supplier inquiries when they should be spending that time on more worthwhile and strategic projects.
Digital payments are among the quickest ways to make payments, which lessens the possibility that suppliers will have to inquire about the status of a transaction. Digital payment solutions offer both parties greater visibility and a more transparent payment timeline than mailing and tracking a physical check. 72% of healthcare teams stated that they would like to make more electronic payments in the upcoming year, which can be explained in part by these advantages.
6. Accelerated Shift Toward Value-Based Reimbursement Models
Value-based care, in which clinicians are compensated for patient outcomes rather than the quantity of services rendered, is the direction that healthcare payments will take in the future. New digital solutions are necessary to facilitate the shift because traditional payment systems aren’t suited for this.
Value-based care is increasingly relying on bundled payments, which provide a single payment for a full course of treatment as opposed to separate fees for each service. This system helps manage resources more effectively while concentrating on patient outcomes by promoting efficiency and cost-effectiveness.
Dealing With Inconsistent Pricing, Manual Data Entry, And High Quote Revisions? Let Artificial Intelligence Software Development Services Solve It
AI Transforming Healthcare Reimbursement Process
AI and automation can streamline healthcare reimbursement by increasing productivity, lowering errors, and ensuring on-time reimbursements. AI is changing the industry in the following ways:
- Automated Claims Processing & Medical Coding: The coding and documentation preparation process is automated by AI-powered platforms, ensuring that claims are clean and prepared for submission to clearinghouses or payers.
- Predictive Analytics for Claim Denials: AI can forecast the probability of claim denials by examining past claims data. This increases the likelihood of a successful healthcare reimbursement by enabling providers to make corrections prior to filing the claim.
- Data Integration Across Platforms: Data from insurance companies, billing systems, and Electronic Health Records (EHR) may all be integrated via AI-driven solutions, ensuring that everyone has access to consistent, real-time data. This lessens back-and-forth communication and enhances coordination.
- Improved Eligibility Verification: Automated systems can promptly confirm a patient’s eligibility for insurance coverage, giving clinicians advance notice of whether services will be paid for. By doing this, rework and reimbursement cycle delays are prevented.
Conclusion
The future of healthcare reimbursement trends will be shaped by automation, digital tools, and a stronger focus on value-based care. Even though challenges such as higher patient payments and complex billing rules continue to grow, they also open the door for better systems. To succeed in 2026 and beyond, providers need clean documentation, smooth workflows, and teams that can adapt to new trends with ease. Simple, fast, and accurate processes will be the key to steady cash flow and fewer payment delays.
NextGen Invent’s digital health software development services help healthcare organizations move in this direction. These solutions support digital workflows, improve data accuracy, reduce manual work, and make the reimbursement process easier for staff and patients.
As payment models evolve, the right technology partner can turn pressure into progress. With NextGen Invent, providers can build strong, reliable systems that support financial stability while keeping patient care at the heart of every decision.
Frequently Asked Questions About Healthcare Reimbursement Trends
Related Blogs
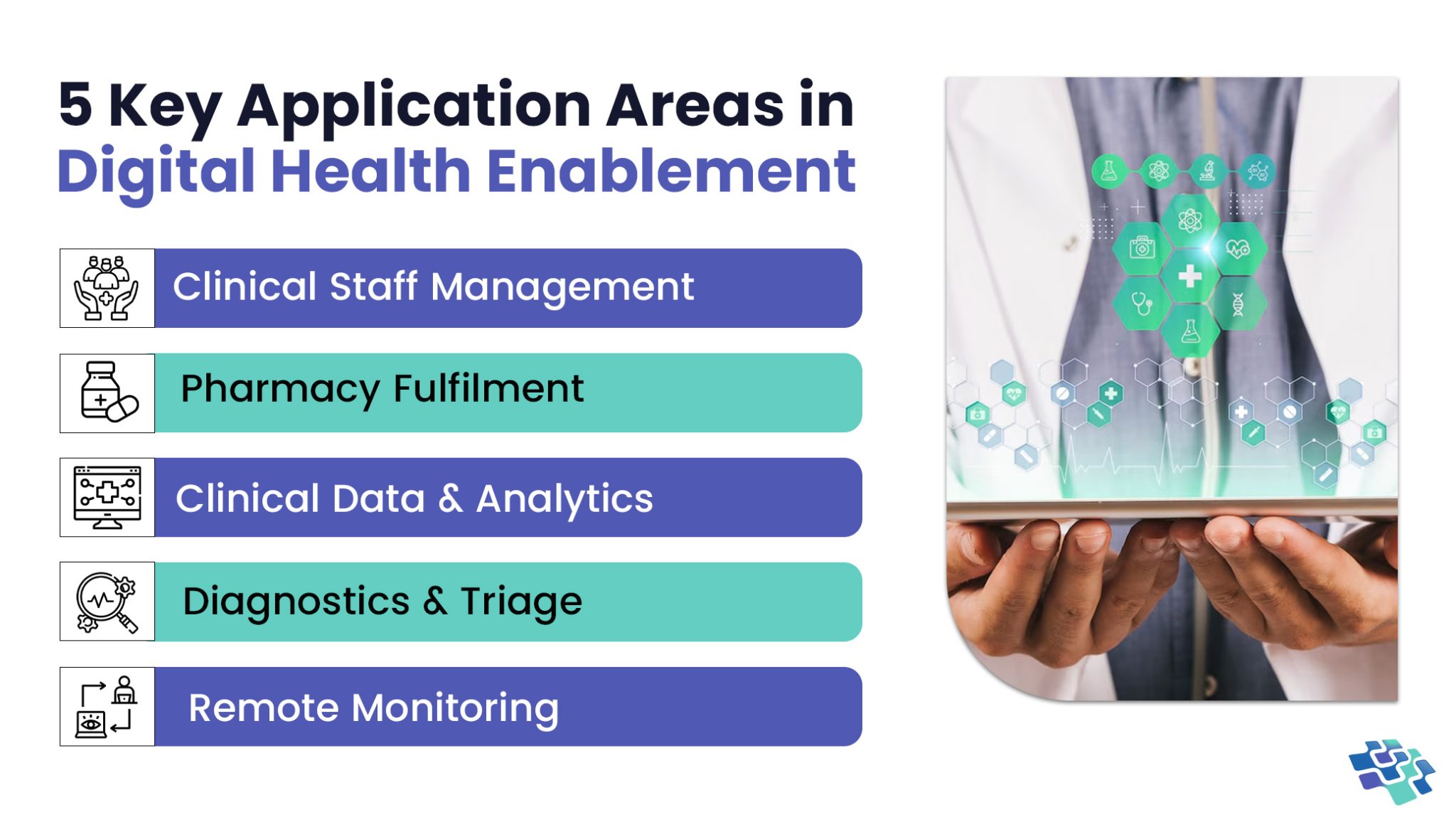
Unlocking Healthcare Innovation through Digital Health Enablement
What defines an effective digital health enablement system? Having quick and easy access to the data you need is undoubtedly important. A few minutes of delay in accessing data could mean the difference...
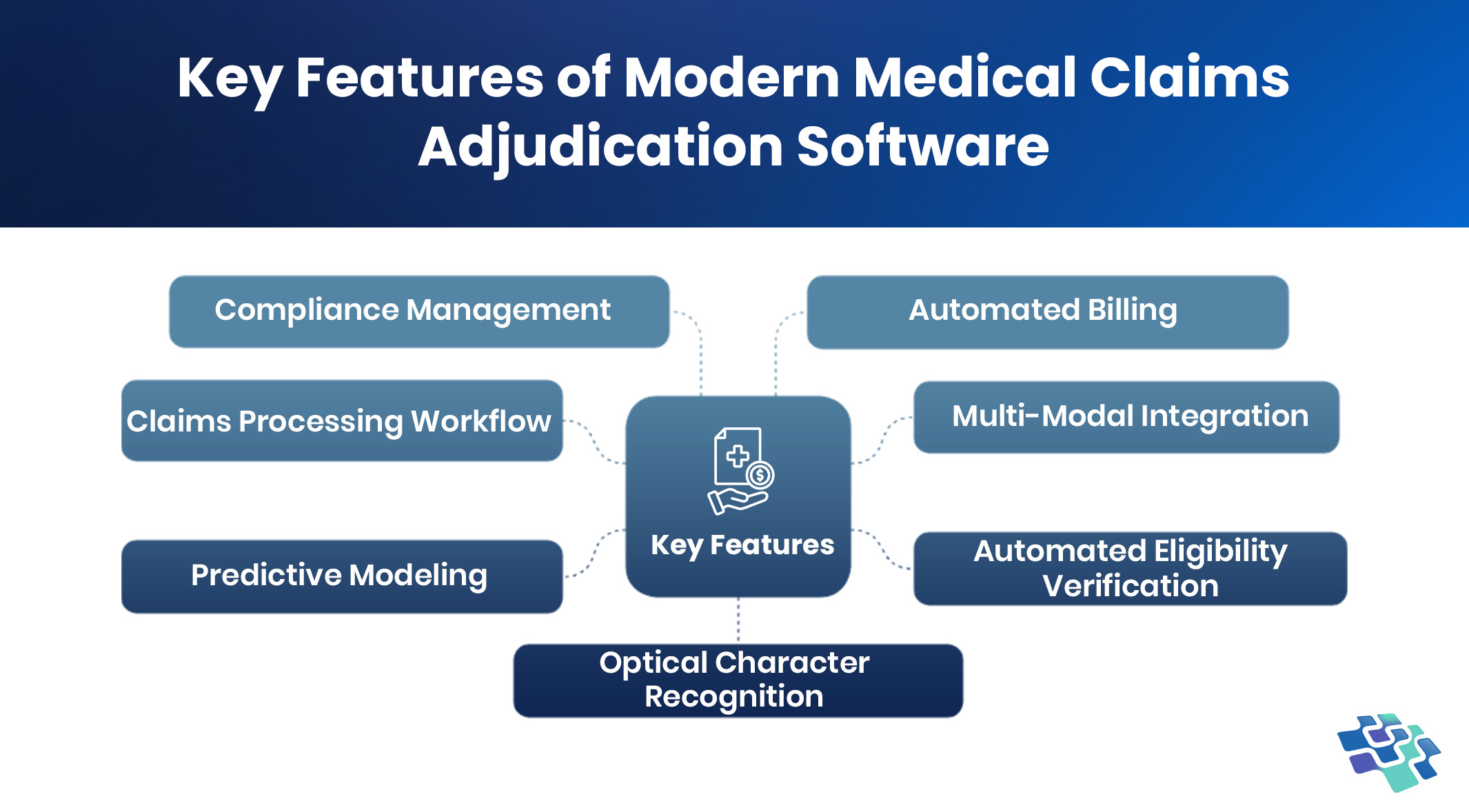
How Augmented Healthcare Claims Adjudication Software Solves the Hidden Crisis in Billing
Is this claim valid? To what extent are we financially responsible? When evaluating medical claims, these are the two main questions that payers try to address.
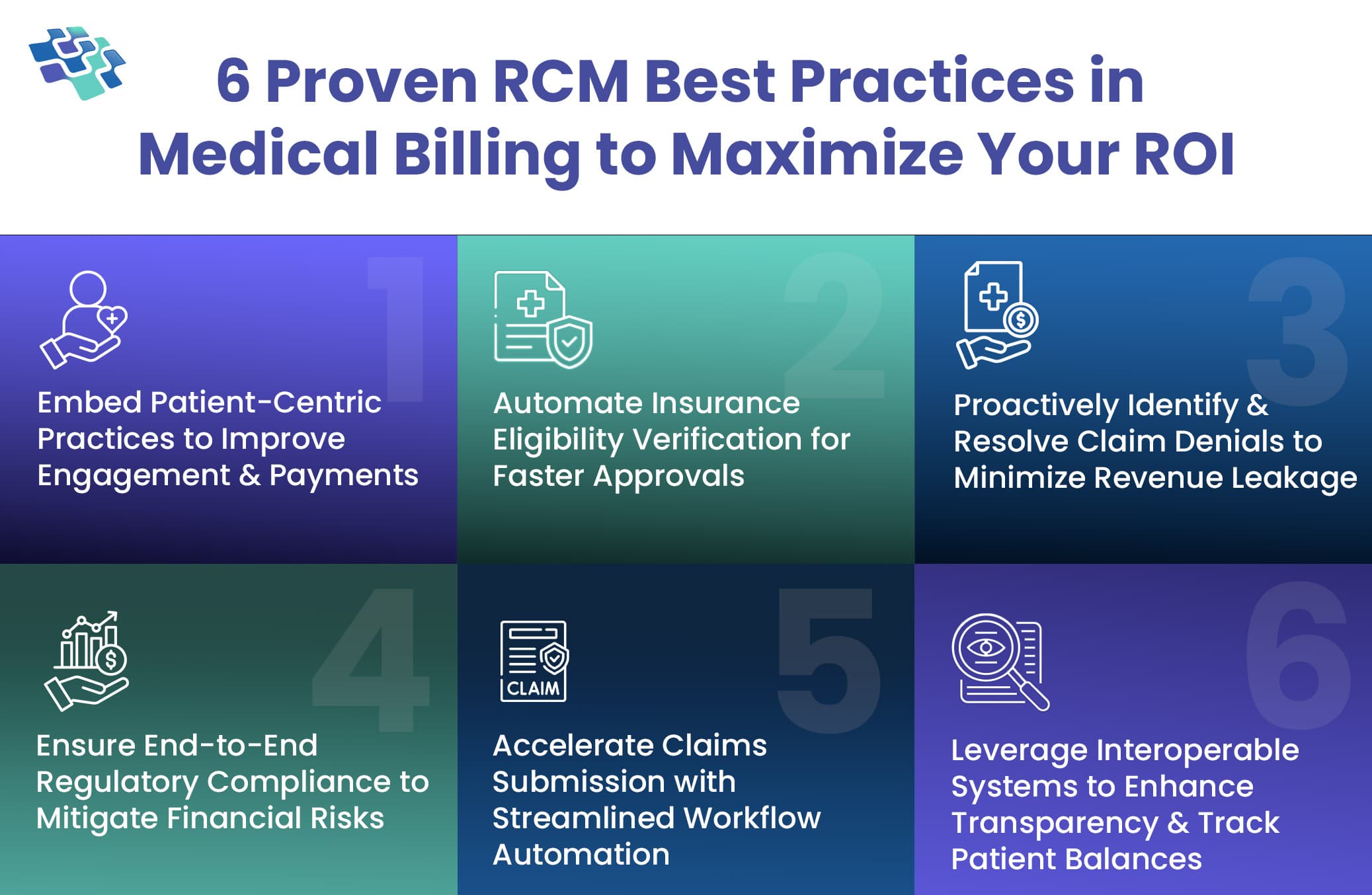
RCM in Medical Billing: Fix Denials, Delays, and Disruptions with These 6 Proven Best Practices
Revenue cycle management is a crucial process in healthcare that governs the financial operations, ensuring providers are accurately compensated for their services. But have you ever wondered...
Stay In the Know
Get Latest updates and industry insights every month.
 1. The Rise of Paperless & Automated Billing Workflows
1. The Rise of Paperless & Automated Billing Workflows