How Augmented Healthcare Claims Adjudication Software Solves the Hidden Crisis in Billing
A potent solution is provided by medical claims adjudication and augmented software. Automating and streamlining the entire claims process helps providers increase accuracy, save time, and receive payment more quickly.

Struggling With Claim Delays? Discover How Our Digital Health Software Development Services Accelerate Adjudication and Reimbursement

“Administrative errors account for 5-50% of medical errors in primary care, recognizing the need for digital accuracy solutions like medical billing and claims processing management, which includes services and software.”– World Health Organization
Augmented Claims Adjudication Explained for Strategic Decision-Makers
It is the procedure for reviewing and handling claims that medical professionals submit to insurance companies to get paid. To ensure correctness and adherence to legal requirements, a comprehensive grasp of healthcare billing codes, policy details, and patient data is necessary.
Health plans and other payers review medical claims submitted by providers during this process and decide whether to pay the claim in full, partially, or reject it completely.
Healthcare professionals must verify patient enrollment, coverage status, and determine if prior authorizations or referrals are required. Skipping this step can lead to claim processing delays and potential revenue loss for providers.
To ensure reimbursement, a claim needs to fulfill the following requirements:
- Providers must confirm patients’ coverage and authorization needs.
- Accurate patient and service information must be included in claims.
- Every document needs to adhere to payer and regulatory standards.
Check our case study: Technical Accelerator Diligence: Future-Proofing a Digital Health Platform
Why The C-Suite Can’t Ignore the Billing Breakdown Anymore
Billing inefficiencies are no longer just an operational issue; they threaten margins, patient satisfaction, and regulatory compliance. For CEOs, resolving this hidden issue is critical to sustaining profitability and achieving long-term strategic growth.
Key risks CEOs must address are:
- Revenue Leakage: Inaccurate adjudication and delayed claims can lead to significant uncollected revenue.
- Operational Drag: Manual workflows increase processing time, inflate costs, and limit scalability.
- Compliance Exposure: Inconsistent billing practices heighten the risk of audits and penalties.
Unlocking Efficiency for Small and Mid-Sized Providers with Augmented Claims Adjudication Software
To manage claims, large hospitals usually have sizable billing departments. Smaller clinics, individual practitioners, and mid-sized healthcare organizations often do not have the same resources. They can handle every facet of patient intake and payment posting with just one person or a small billing team.
Healthcare claims adjudication and augmented software are essential for smaller providers for the following reasons:
- Limited Staff: Claims automation eases the workload for small teams.
- Cash Flow Dependence: Delays in payments are frequently unaffordable for smaller providers.
- High Error Risk: Manual procedures result in more errors and denied claims.
- Administrative Overload: Providers should prioritize patient care over paperwork.
- Compliance Pressures: HIPAA and other regulations demand that patient data and claims be handled carefully.
Key Challenges of Adjudication in Medical Billing and Ways to Tackle Them
The adjudication of medical claims is a complicated process with multiple challenges. Clinics must deal with them if they wish to process claims accurately and quickly.
- Eligibility Verification Issues: Claims can be denied because of the long and error-prone process of determining a patient’s eligibility for care. This can be fixed by using systems that immediately search insurance databases to determine a patient’s eligibility. To prevent confusion and ensure a seamless verification process, keep patient and insurance information updated.
- Denial Management: It takes time to handle claims that are rejected. After determining the reason for their denial, businesses must correct the mistakes and resubmit them. To monitor the reasons for the denial of claims and to streamline the process, it is advisable to employ denial management solutions.
- High Volume of Claims: Managing numerous claims can strain your staff, leading to mistakes and delays. Utilize scalable software to handle claims to prevent this. Batch processing can reduce human labor and simplify repetitive activities for your staff.
- Complex Medical Policies: It can be quite difficult to deal with insurance regulations, which might result in non-compliance and denied claims. Use rule-based medical claims adjudication and augmented software, and train your employees in the most recent payer rules and healthcare legislation to keep them updated.
Benefits of Augmenting Medical Claims Adjudication Software
The goal of implementing healthcare claims processing software is to change how your company manages each stage of the claims process, not just automate it. From quicker approvals to fewer mistakes, the correct solution produces quantifiable gains in operations, finance, and customer service.
- Accelerated Claim Resolution Times: Processing time is reduced by automating every stage of the claims process, from input to settlement. Software for processing claims expedites the workflows for document capture, eligibility verification, and approval, ensuring quicker results. By eliminating human data entry and facilitating real-time decision-making, the software can reduce time-to-decision with AI-powered document recognition.
- Reduced Operational Costs & Manual Labor: Augmenting the claims adjudication system lowers overhead expenses and eliminates the need for large processing teams by automating repetitive administrative procedures. Modern solutions reduce the cost per claim by up to 80% by eliminating manual input. Teams can accomplish more with fewer resources because of centralized dashboards, batch processing, and smart routing.
- Better Compliance & Risk Management: Most claims adjudication software solutions come with compliance features, including HIPAA, GDPR, and local insurance regulations. Automated documentation, audit trails, and access controls make it easier for businesses to maintain compliance.
- Improved Accuracy & Reduced Errors: In manual claims processing, human error may result in rework, hold-ups, and rejected reimbursements. By ensuring consistent data capture, validation, and compliance checks, healthcare claims adjudication and augmented software increase accuracy.
Accelerate Payment Processing and Minimize Denials Through Advanced Claims Automation and Integration Capabilities
How Today’s Augmented Healthcare Claims Adjudication Software Works Smarter
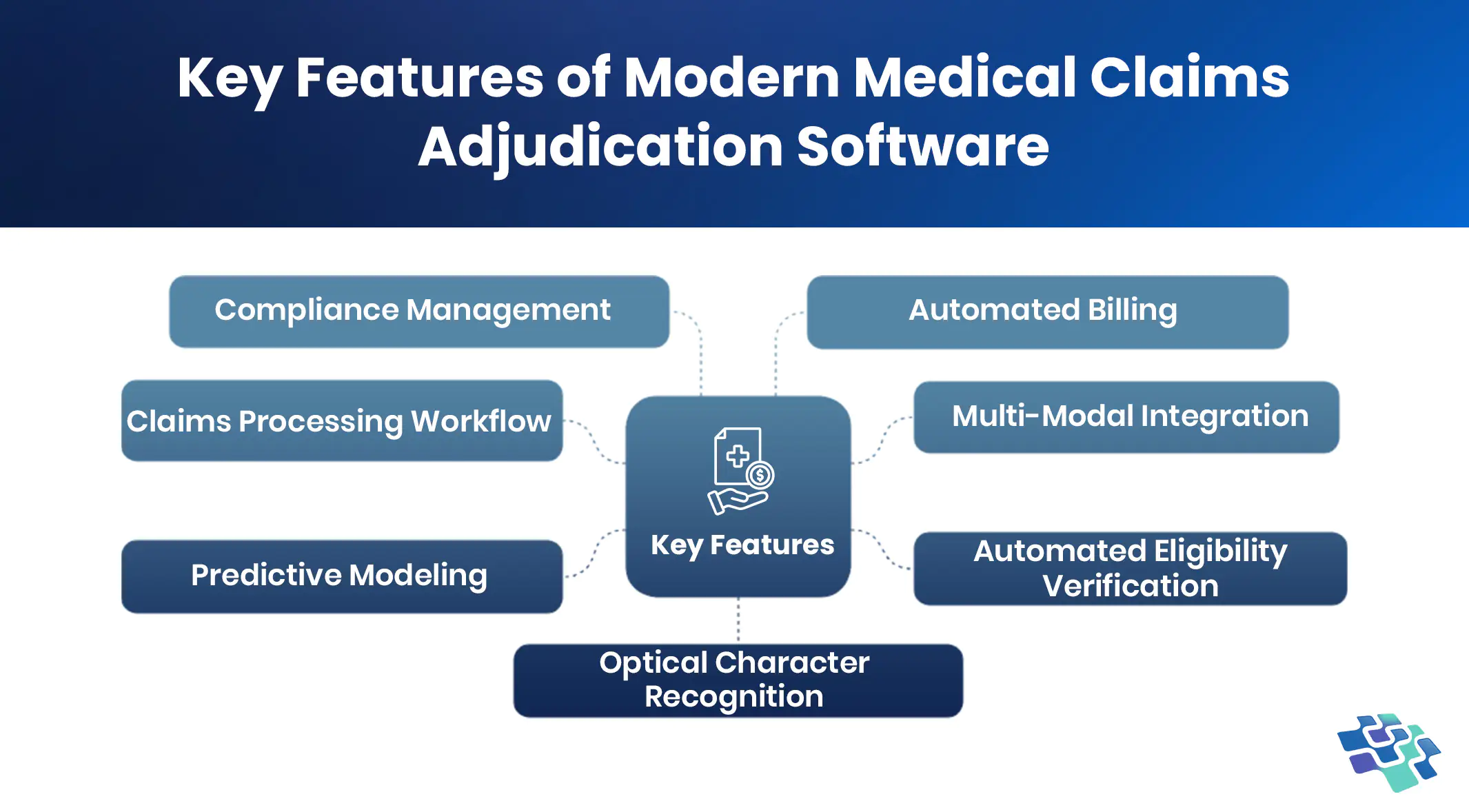
The medical claims adjudication software analyzes claims data and decides how to handle each claim differently by combining AI, machine learning, and established rules. It also automates requests for more details or clarification on claims and correspondence between payers and providers. The healthcare claims adjustment software has the following key features:
 1. Compliance Management
1. Compliance Management
In medical claims software, compliance management refers to the procedures and frameworks that ensure healthcare providers follow all the regulations and guidelines that control the healthcare sector. This entails keeping correct records, appropriate coding processes, and safeguarding patient data in accordance with regulations like HIPAA. For healthcare providers, maintaining compliance with healthcare standards is crucial because it protects them from financial penalties and legal repercussions for non-compliance.
Medical claims adjudication and augmented software must have several crucial features to implement compliance management effectively. Automated compliance checks are crucial because they keep an eye on claims to make sure they follow billing regulations, coding standards, and documentation specifications. By identifying potential problems before claims are filed, these checks enable providers to proactively fix mistakes.
2. Automated Billing
The creation, processing, and tracking of invoices and payments are managed by an automated billing system in medical claims software, which eliminates the need for human involvement. The first of its many noteworthy benefits is that it significantly lowers the possibility of errors that are frequently made in manual billing procedures, like inaccurate amounts, missing patient data, or coding problems. Denials of claims and overdue payments brought on by mistakes can have a detrimental effect on a healthcare practice’s revenue flow.
Healthcare providers can save valuable time by automating tasks, which frees up administrative staff to focus on other crucial duties. Automated billing procedures also simplify invoicing, which speeds up reimbursement and improves cash flow. Providers can effectively manage operations and focus resources toward providing high-quality patient care because of their financial stability.
To lower the risk of past-due payments, automated billing should be able to remind patients and insurance companies when payments are due, based on due dates and outstanding balances. Reducing inconsistencies and the need for manual data entry, seamless connection with Electronic Health Records (EHR) systems ensures that all relevant patient and service information is appropriately recorded and represented in bills.
3. Claims Processing Workflow
A key element of healthcare financial management that ensures effective, safe, and legal operations is the claims processing workflow. Workflow management technologies developed for claim processing are engineered to streamline each stage, from claim development to submission and follow-up, optimizing the flow of tasks and boosting productivity. Because of the great degree of configurable nature of these workflow management solutions, healthcare organizations can customize the claims processing processes to meet their unique requirements.
This customization can involve specifying the order of processes, automating specific actions according to preset guidelines, and configuring alerts for occasions or turning points in the claim’s lifetime. Through workflow customization to the specific procedures of the company, these technologies reduce bottlenecks and expedite the claims process through the system.
To ensure accountability and transparency, these workflow technologies’ integrated audit trails and reporting features are essential. Every action related to a claim is tracked by audit trails, which offer a thorough record of who did what and when. This degree of traceability is essential for compliance and audit preparation and helps determine the causes of mistakes or delays. However, reporting functions provide information about how productive and efficient the workflow is for processing claims.
4. Multi-Modal Integration
Patients, insurance companies, and healthcare providers can all be connected via a dependable and secure platform provided by strong augmented healthcare claims adjudication software. It is possible to design the medical claims adjudication process to provide many access channels, immediate claims checks, and validation in a completely automated and paperless setting by gaining access to electronic health systems.
Augmented claims adjudication software can integrate medical claims, prevent work duplication, and improve the efficiency of your patient accounting system by utilizing cloud computing in the healthcare industry. File sharing, smart edit embedding into EMR, upstream content distribution, and other features are all included in multi-modal integration. The last component of automated medical claims adjudication is carrier-specific data in automatic worklists, detailed procedure codes, and flagged claims.
5. Predictive Modeling
Predictive modeling that promotes steady cash flow and helps predict future revenue streams can be provided by healthcare automation. The patient’s eligibility and pre-authorization verification prior to the examination can be used to creatively design automated claim adjudication in medical billing to increase revenue collection. This produces an unparalleled level of transparency by means of web-based performance management tools and thorough claims reporting.
Using monthly eligibility and capitation lists, clinical informatics systems help reduce claim denials and write-offs. Automating reporting, capture, auditing, and communication enables “touchless” claims adjudication without manual intervention, improving efficiency and consistency across the medical billing process.
6. Automated Eligibility Verification
Automated eligibility verification helps verify patient eligibility and determine appropriate coverage for each claim. It evaluates the patient’s insurance coverage for the requested services and provides real-time eligibility status. This feature minimizes the risk of submitting claims for non-covered services and helps prevent future claim denials.
By automating these verification steps, the software significantly reduces administrative workload. This allows staff to focus more on key tasks such as improving patient care, enhancing patient satisfaction, and managing practice operations more efficiently.
7. Optical Character Recognition
Augmented claims adjudication software must continuously evolve to enhance satisfaction across all stakeholders in the healthcare ecosystem. A key feature supporting this evolution is Optical Character Recognition (OCR), which significantly reduces the risk of coding and filing errors by scanning, digitizing, and isolating data from documents with precision.
From enabling seamless electronic data exchange via mHealth platforms to validating information through advanced technology and flagging errors before submission, these tools offer substantial advantages. Every tailored claims management solution boosts retention rates, increases revenue, and streamlines the entire claims lifecycle through automation and intelligent health system integration.
Boost Reimbursement Rates and Reduce Processing Time with Intelligent Digital Claims Processing Tools
How to Enhance Accuracy and Reduce Delays in Claims Adjudication
The financial consequences make it imperative that providers continually submit “clean” claims. Accurate information about the patient, diagnosis codes, file types, and submission dates must all be included in the claim. Here are five crucial tactics that medical facilities can use to lighten their administrative workload and speed up the claims adjudication procedure:
- Invest In Automation
Automation can save healthcare providers time and reduce costs, with electronic claim submissions potentially saving $1.7 billion annually. Automated workflows speed up adjudication, reduce errors, and enhance decision-making. Payers benefit from interoperable data, while clinicians avoid duplication, verify patient details, track policy changes, and assign tasks more efficiently.
- Efficient Data Management
Claim rejections often result from inaccurate or inconsistent patient data, such as name mismatches on discharge forms. Electronic medical records linked by a Universal Patient Identifier (UPI) reduce these errors, enabling real-time visibility. Automated workflows and trackers help staff monitor claims, manage denials, and stay updated throughout the adjudication process.
- Enhance Patient Communication
While providers must verify patient information, patients also play a key role in avoiding claim delays by sharing accurate, timely details. As digital registration grows, each online touchpoint becomes a chance to confirm data accuracy. Strengthening patient-provider collaboration is essential for streamlining and optimizing the claims adjudication process.
- Standardize Claims Adjudication
Standardizing the claims adjudication process brings consistency across operations, reducing uncertainty for healthcare providers. It helps minimize errors, accelerate claim turnaround times, and boost overall efficiency. As a result, providers benefit from improved cash flow, greater operational stability, and enhanced potential for long-term business growth in a competitive environment.
Check our case study: AI Labeling & Safety Automation: Revolutionizing Regulatory Affairs, Compliance, Reducing Time, and Fueling Unstoppable Growth
Why It’s Time to Rethink Your Claims Adjudication Process
It may be time to explore more intelligent options if your company still relies heavily on manual processes. In addition to negatively affecting your cash flow, delays, mistakes, and denials also impact client satisfaction and operational effectiveness.
This is where the use of augmented claims adjudication software can have a discernible impact.
With a claims adjudication and augmented software, businesses can:
- Reduce claim errors and reprocessing
- Accelerate reimbursement cycles
- Leverage analytics to forecast claim outcomes
- Enhance precision with automated rules
- Enable smooth integration with current systems
Conclusion
Healthcare reimbursement is inherently complex, requiring precision at every stage of the claims lifecycle. Leading healthcare organizations understand that excellence in claims adjudication isn’t just about recovering revenue; it’s about building efficient, accurate systems that support better patient outcomes and long-term financial sustainability.
To stay competitive, providers and payers must invest in advanced technology, continuous staff training, and seamless cross-functional workflows. As the industry evolves, those who embrace automation and data-driven decision-making will be best positioned to improve reimbursement speed, accuracy, and overall operational performance.
NextGen Invent’s AI-based provider operations software development services empower healthcare organizations to reduce errors, accelerate decision-making, and ensure accurate payments. With intelligent automation, real-time validation, and configurable rule engines, the platform streamlines the adjudication process and removes guesswork from claims review.
Ready to transform your claims process?
Schedule a demo with NextGen Invent and discover how we can help you reduce turnaround time, minimize denials, and boost claims adjudication success.
Frequently Asked Questions About Augmented Healthcare Claims Adjudication Software
Related Blogs
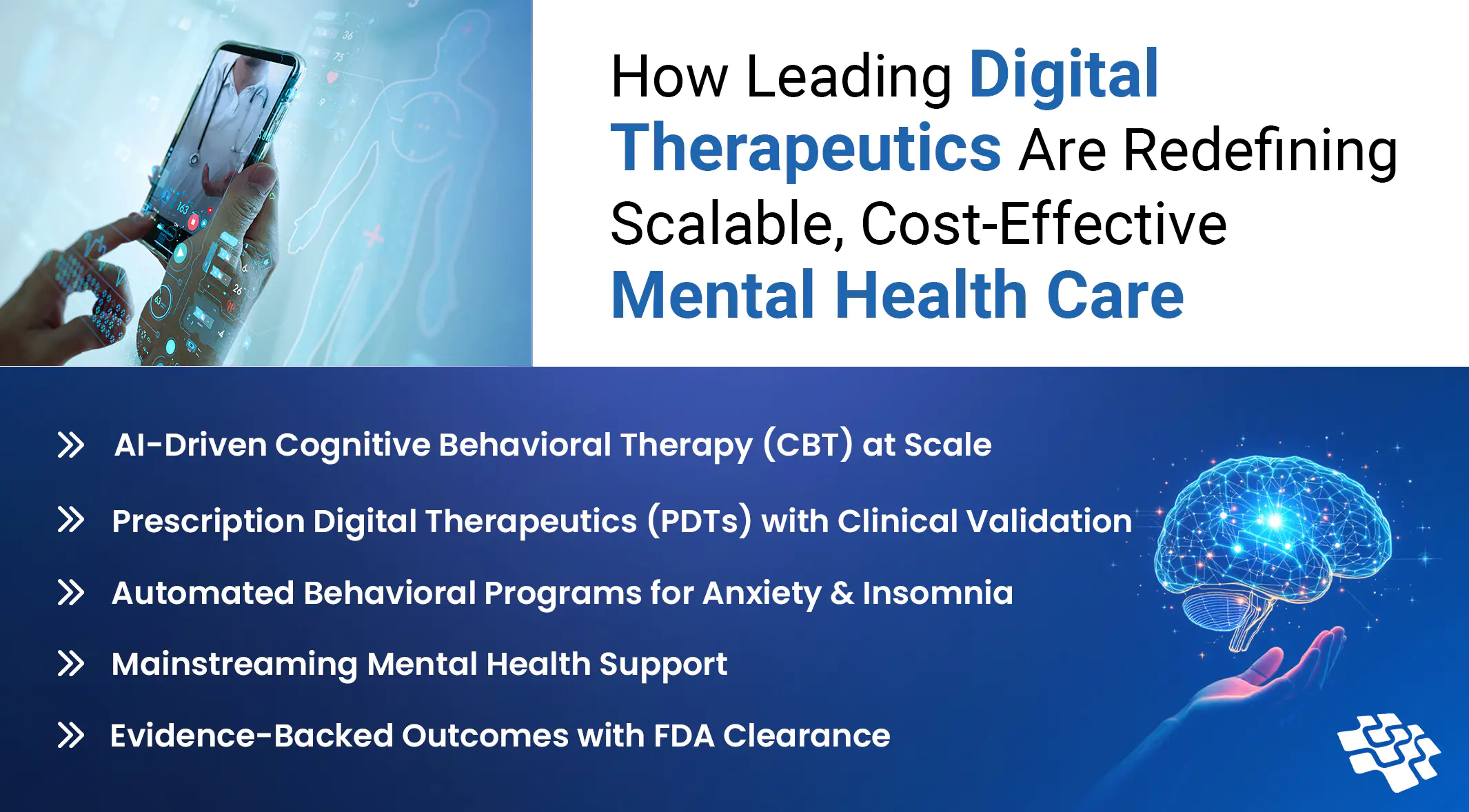
Digital Therapeutics for Mental Health - How Technology is Shaping the Future Well-Being
The field of digital mental health has expanded significantly in the last ten years, covering a wide range of areas such as digital therapeutics for mental health, personalized medicine, telehealth and telemedicine, and mobile health.
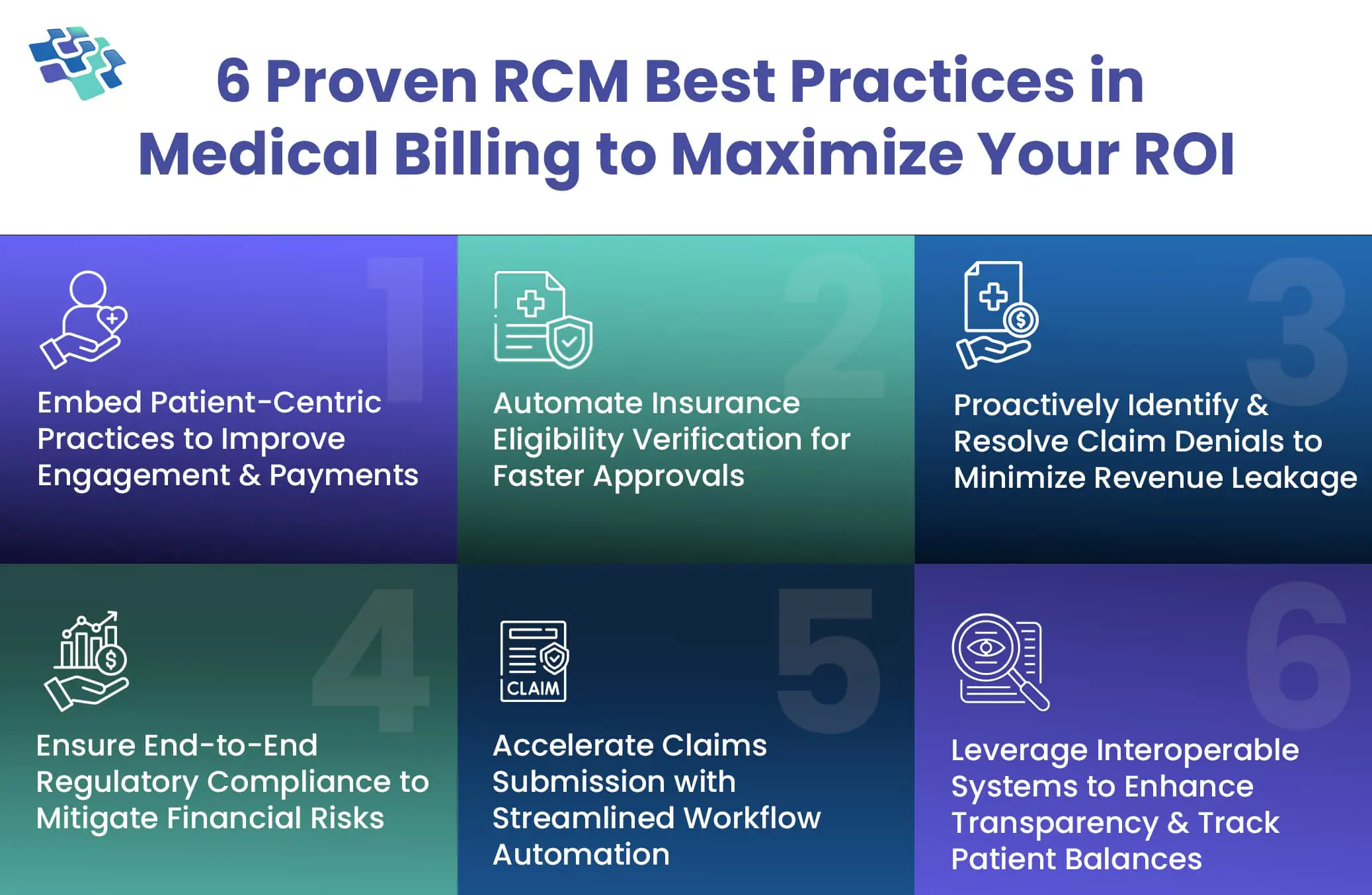
RCM in Medical Billing: Fix Denials, Delays, and Disruptions with These 6 Proven Best Practices
RCM in healthcare involves managing everything from patient registration and insurance verification to claim submission, payment collection, and revenue generation.
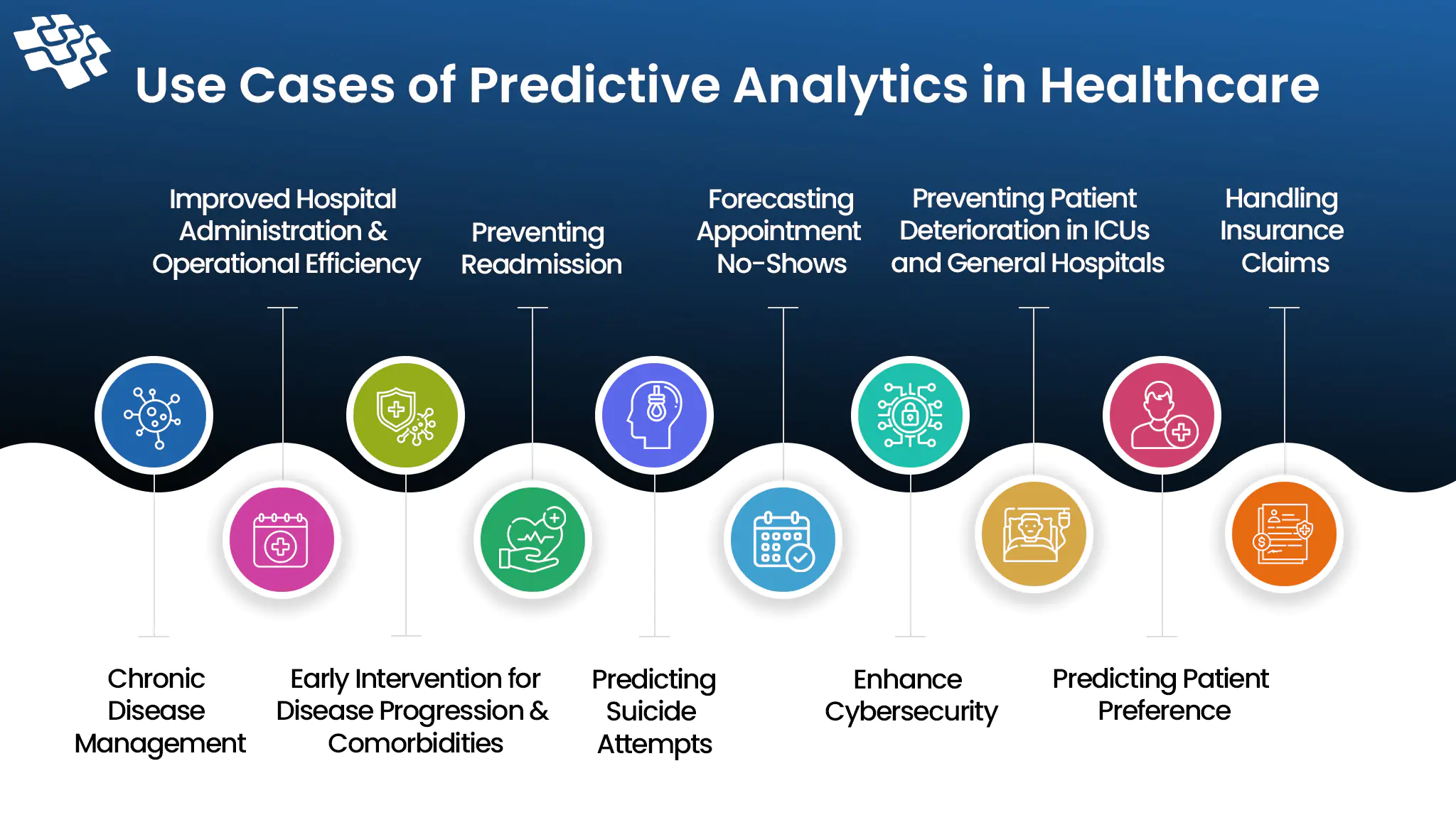
How is Predictive Analytics in Healthcare Revolutionizing It?
Predictive analytics in healthcare is real and not just science fiction. Better patient care and early intervention are made possible by predictive analytics, which forecast health outcomes using advanced analytics tools and healthcare data.
Stay In the Know
Get Latest updates and industry insights every month.
 1. Compliance Management
1. Compliance Management