Importance of EHR Integration for Your Virtual Care
- 74% of physicians provide remote services in their practices.
- 88.2% of office-based physicians now utilize electronic health records.
EHR and remote patient monitoring software development are frequently kept apart and not integrated. Healthcare providers can ensure efficient healthcare service delivery, lower professional burnout, and improve access to care by integrating a virtual care platform with an EHR system.

Having Trouble Managing Patient Data? Our EHR Integration Simplifies Record Handling and Boosts Efficiency
“Integrating EHR systems into the healthcare workflow enhances the accuracy of billing processes and revenue cycle management, leading to cost savings. As healthcare providers navigate the complexities of the modern healthcare landscape, the financial gains derived from efficient EHR utilization become critical in sustaining and advancing healthcare services.”– Research Gate
Overview of Virtual Care Management Program
Virtual care management solutions are now the industry standard for managing chronic conditions and facilitating ongoing patient care. These programs enhance patient outcomes, expand access to care, and reduce healthcare costs by utilizing digital technologies. Programs for virtual care management fall into three primary categories:
- Remote Patient Monitoring: Through digital technology and networked medical devices, remote patient monitoring software collects and transmits patient health data to healthcare providers in near real-time. Continuous monitoring, data transmission, and improved results are some of RPM’s primary characteristics.
- Chronic Care Management: The goal of chronic care management is to coordinate treatment for those who have several chronic illnesses. It seeks to improve patients’ health outcomes by offering all-encompassing care and resources. Regular follow-ups, patient education, and care coordination are important components of CCM.
- Principal Care Management: Patients with a single chronic disease that needs continuous care management are the focus of principal care management. Focused management, improved access, and EHR integration are crucial elements of PCM.
What Does EHR Integration Achieve?
Quick access to medical records through the integration of your EHR and practice management system enables more effective diagnosis and treatment. Additionally, patients can electronically enter their personal information, which speeds up and improves the effectiveness of onboarding. Additionally, you can complete tasks like online scheduling that your conventional EHR system does not offer.
Through an EHR integration, information is shared, including patient demographics, medical history, prescription drugs, allergies, and test results.
Additional advantages consist of:
- Instant access to current, validated patient data without delay.
- Effortless EHR storage, management, and sharing among healthcare providers.
- Enhanced efficiency through streamlined administrative and clinical workflows.
Challenges That Organizations Might Face During EHR Integrations
EHR integration could face the following technical challenges:
- Issues in Interoperability: A lack of standardization could make it challenging to communicate data seamlessly.
- Challenges in API Configuration: Setting up APIs might be challenging for companies with little IT resources.
- Workflow Challenges: A new system’s integration may cause your current workflow to change. EHR connections can result in more paperwork duties for medical professionals.
- Complexity in Data Mapping: Inconsistencies and mistakes can result from data structure mismatches.
Best Practices for Successful EHR Integration
It takes careful planning, collaboration, and adherence to the best standards to integrate virtual care features into Electronic Health Record software. Follow these recommendations to make sure the integration process goes well:
- Define Clear Goals
- Involve Key Stakeholders
- Develop a Comprehensive Plan
- Select the Right Virtual Care Platform
- Verify System Compatibility
- Offer Thorough Training
- Track Performance and Results
Struggling with Disconnected Systems? Our EHR Integration Ensures Seamless Data Access for Virtual Care
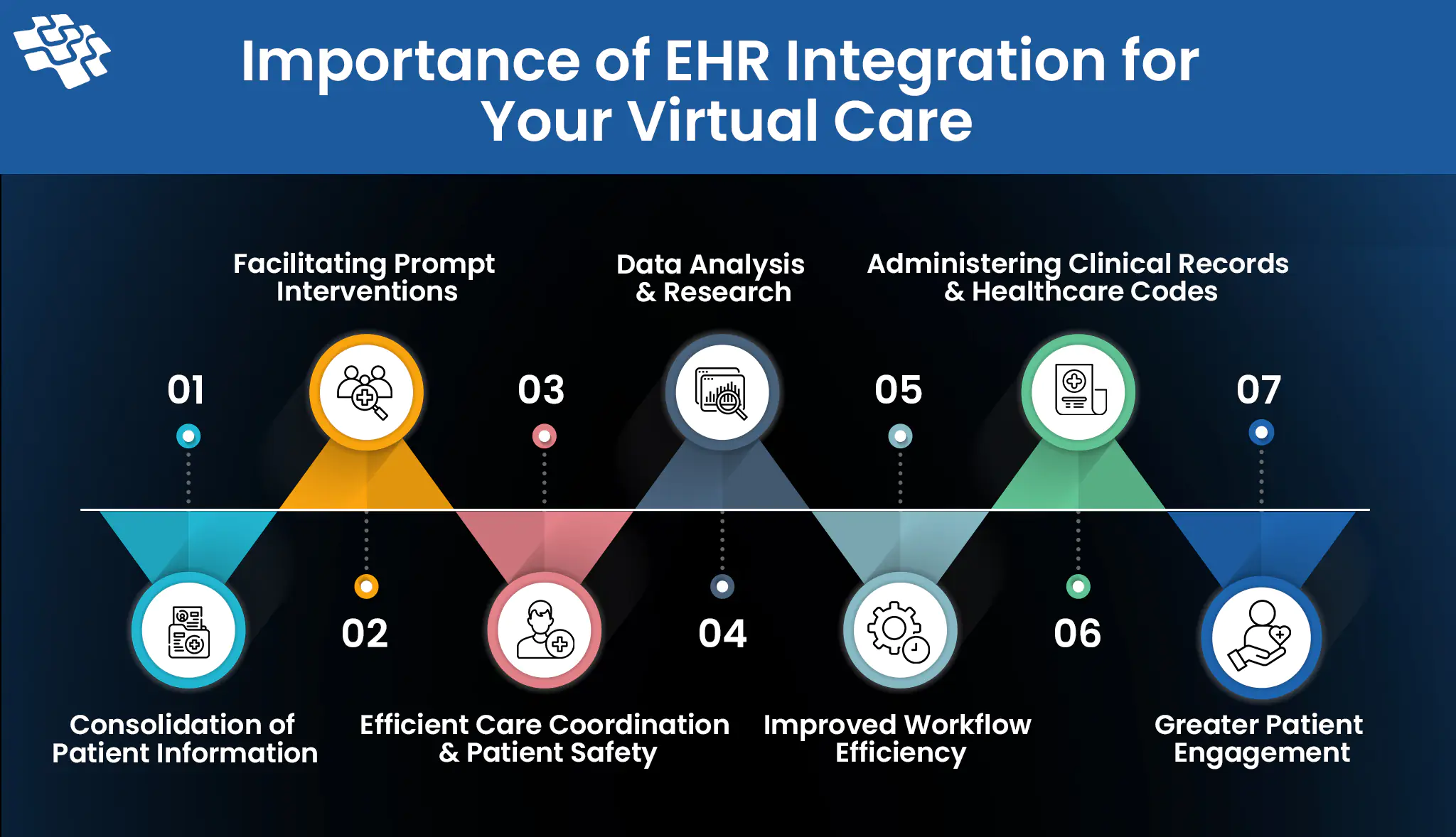
Importance of EHR Integration for Your Virtual Care
EHR integration is essential for effective virtual care, enhancing data access, decision-making, and patient outcomes. Below are 7 key reasons why integrating EHR with virtual care strengthens healthcare delivery and efficiency.
 1. Consolidation of Patient Information
1. Consolidation of Patient Information
Patient data from multiple sources is combined into a single, cohesive record through EHR integration. Information from the following sources is included in this consolidation:
- Different Healthcare Providers: It is possible to combine patient data from several providers—such as hospitals, primary care doctors, and specialists—into a single, easily accessible EHR. Care coordination requires this comprehensive approach, particularly for individuals with complicated medical conditions.
- Remote Monitoring Devices: The EHR allows for the immediate uploading of data from wearable technology and remote monitoring technologies, giving medical professionals access to the most recent health trends and indicators.
- Patient-Generated Health Data: Through patient portals or health applications, patients can provide their data. Clinical evaluations gain important context from this patient-generated data.
2. Facilitating Prompt Interventions
Sharing data in near real-time improves care team communication, which supports:
- Patient Engagement: Patients can also be involved in their care through near real-time data exchange. For example, patients can receive warnings to take appropriate action or seek care when their health metrics fall outside of permissible ranges.
- Coordinated Care Efforts: All members of the care team can be promptly informed of changes in a patient’s condition or treatment plan by providers, ensuring that everyone agrees and can respond appropriately.
Reshaping Patient Engagement and Remote Patient Monitoring
3. Efficient Care Coordination & Patient Safety
Care coordination between healthcare providers is improved when virtual care relates to EHR. It enables primary care doctors, specialists, and other medical professionals involved in the patient’s care to securely share test results, treatment plans, and patient information. Everyone engaged will have access to the latest patient data because of this improved communication, which also fosters teamwork.
By lowering the possibility of medical errors, virtual care integration with EHR contributes to increased patient safety. Healthcare professionals can check current prescriptions, confirm medication allergies, and make sure new therapies or prescriptions are safe and suitable when they have access to all patient records. Additionally, this integration facilitates the precise recording of virtual care interactions, ensuring an extensive and current medical record.
4. Data Analysis & Research
Integrating EHRs with virtual care allows healthcare systems to gather valuable data for research and analysis, enhancing patient care and overall system efficiency. By leveraging aggregated and de-identified patient information, healthcare providers can identify trends, assess outcomes, and evaluate treatment effectiveness. This data-driven approach supports continuous improvement in healthcare services, medical procedures, and population health management strategies.
Through this integration, health systems gain insights that help refine patient treatment plans, drive innovation, and improve healthcare outcomes across diverse populations.
5. Improved Workflow Efficiency
Providers can lessen administrative hassles and optimize workflows by integrating telemedicine with EHR systems. A single platform manages billing, documentation, and appointment scheduling, cutting down on errors and duplication of effort.
- Automated Scheduling: The EHR system allows patients to make virtual appointments directly, doing away with the necessity for manual scheduling and lowering the possibility of scheduling conflicts.
- Simplified Billing: Through the linked EHR system, telemedicine or virtual care services can be immediately paid, ensuring prompt and precise reimbursement for physicians.
6. Administering Clinical Records & Healthcare Codes
Managing clinical records can be challenging, but the EHR system streamlines the process, making it easier to maintain accurate healthcare records. This system’s unique functionalities ensure clear, precise, and error-free information, improving data quality and reliability. With the capacity to store vast amounts of information, EHR uses automation tools to logically filter and organize data, minimizing manual effort and enhancing workflow. It supports critical medical decision-making, from treatment plans to financial and inventory-related choices, while also enabling rapid responses in emergencies.
For every medical institution, healthcare coding is essential. Furthermore, this is the primary reason for fines. EHR solutions are essential for minimizing legal actions and lowering medical expenses. In a similar vein, this system shields against online attacks and protects patient data. The following are just a few of the countless benefits of following healthcare codes:
- Generates accurate billing documents
- Standardizes record management
- Reduces liability for healthcare providers
7. Greater Patient Engagement
Patient engagement is fueled by the integration of electronic health records. Patients can take more ownership of their health information and become more involved in their care because of EHR integration. Patients typically have less anxiety and don’t have to wait to see a doctor to view their medical information when they are more involved in their care. Because they are actively participating in their care, engaged patients also have better health results.
Practices looking to increase patient participation and give individuals more control over their health can benefit from integrating electronic health records.
Facing Data Accuracy Issues? Our Services Provide Error-Free, Real-Time EHR Integration for Better Care
Future Trends in Virtual Care EHR Integration
Several upcoming trends are anticipated to influence the virtual care EHR integration landscape as technology develops further.
- AI & Machine Learning in EHR: It is anticipated that virtual care EHR integration will heavily rely on artificial intelligence and machine learning. Predictive analytics, process automation, and increased diagnosis accuracy are all possible with these technologies, which could lead to better patient outcomes.
- The Role of Big Data and Analytics: Improvements in virtual care EHR integration will be fueled by big data and analytics. Large-scale dataset analysis skills can help support evidence-based decision-making, enable preemptive interventions, and offer insightful information on patient populations.
- 5G on Virtual Care EHR Integration: The integration of virtual care EHRs is about to transform with the arrival of 5G technology. Healthcare providers can carry out high-definition video consultations, send real-time patient data, and provide remote monitoring solutions with minimal latency if they have faster and more dependable network connectivity.
Our Expertise & Experience
At NextGen Invent, we offer advanced EHR integration and digital health software development services tailored to meet the evolving needs of healthcare providers. Our team specializes in creating high-quality telemedicine software solutions that ensure seamless, secure access to electronic health records from any device, empowering clinicians to deliver efficient, connected care. With expertise in Artificial Intelligence software development services, we integrate custom AI development solutions to enhance telemedicine platforms, providing valuable data insights, optimizing workflows, and streamlining patient interactions.
Our team has extensive experience and a deep understanding of industry best practices, delivering exceptional results for our clients. Whether it’s enhancing virtual care with robust EHR integration or implementing AI-driven analytics to support clinical decision-making, we’re dedicated to building telemedicine solutions that improve patient care and operational efficiency. Start transforming your virtual care services with our custom AI development solutions and experience the future of healthcare with NextGen Invent.
Frequently Asked Questions About EHR Integration for Your Virtual Care Management
Related Blogs
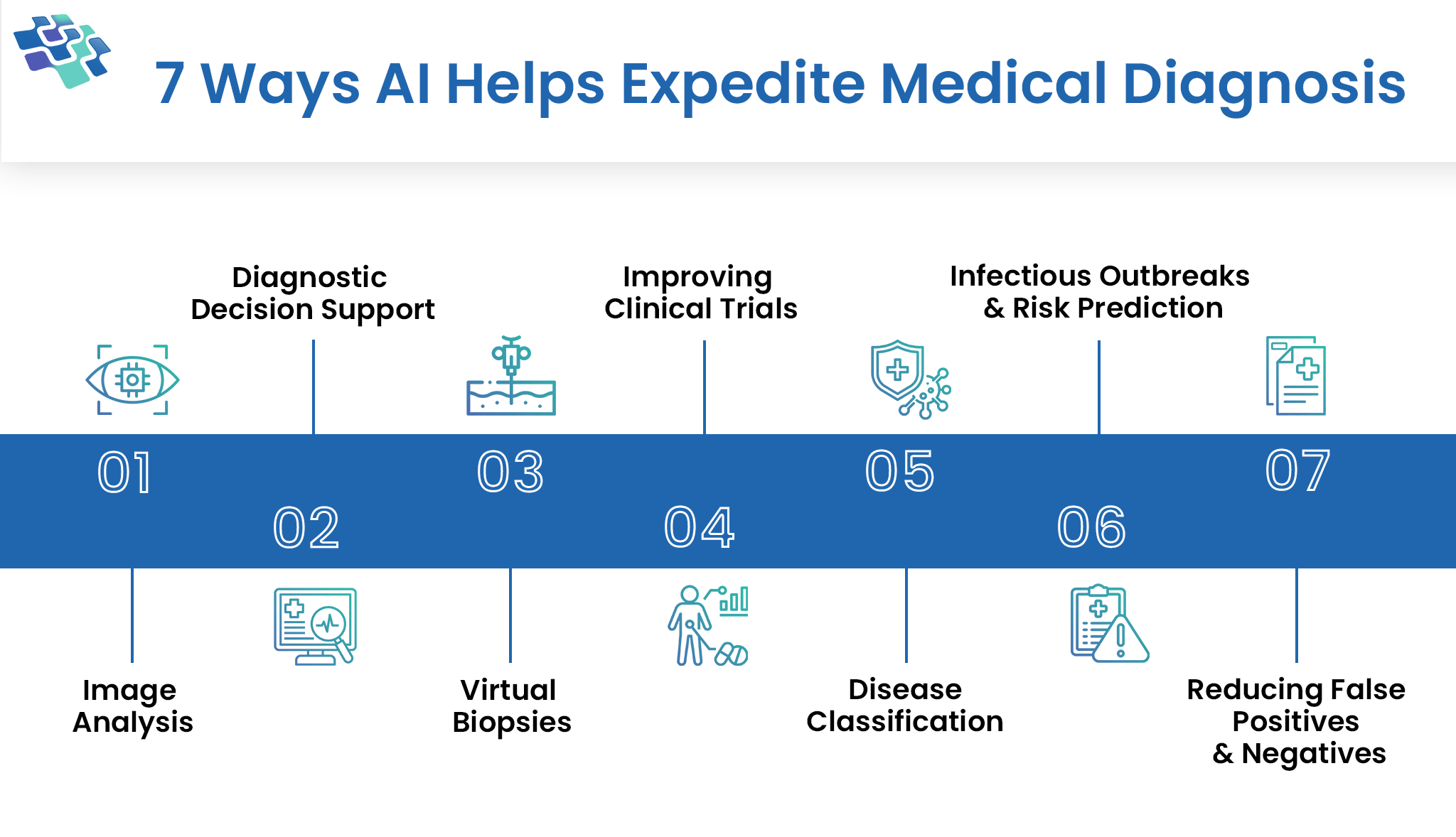
How Does AI in Medical Diagnosis Expedite It?
One of the most noteworthy developments in the healthcare industry in recent years has been the use of AI in medical diagnosis and treatment choices.

Everything Businesses Need to Know About Telemedicine App Development
There will soon be a severe physician shortage in the United States. There is projected to be a 46,900–121,900 physician shortage by 2032. According to estimates...
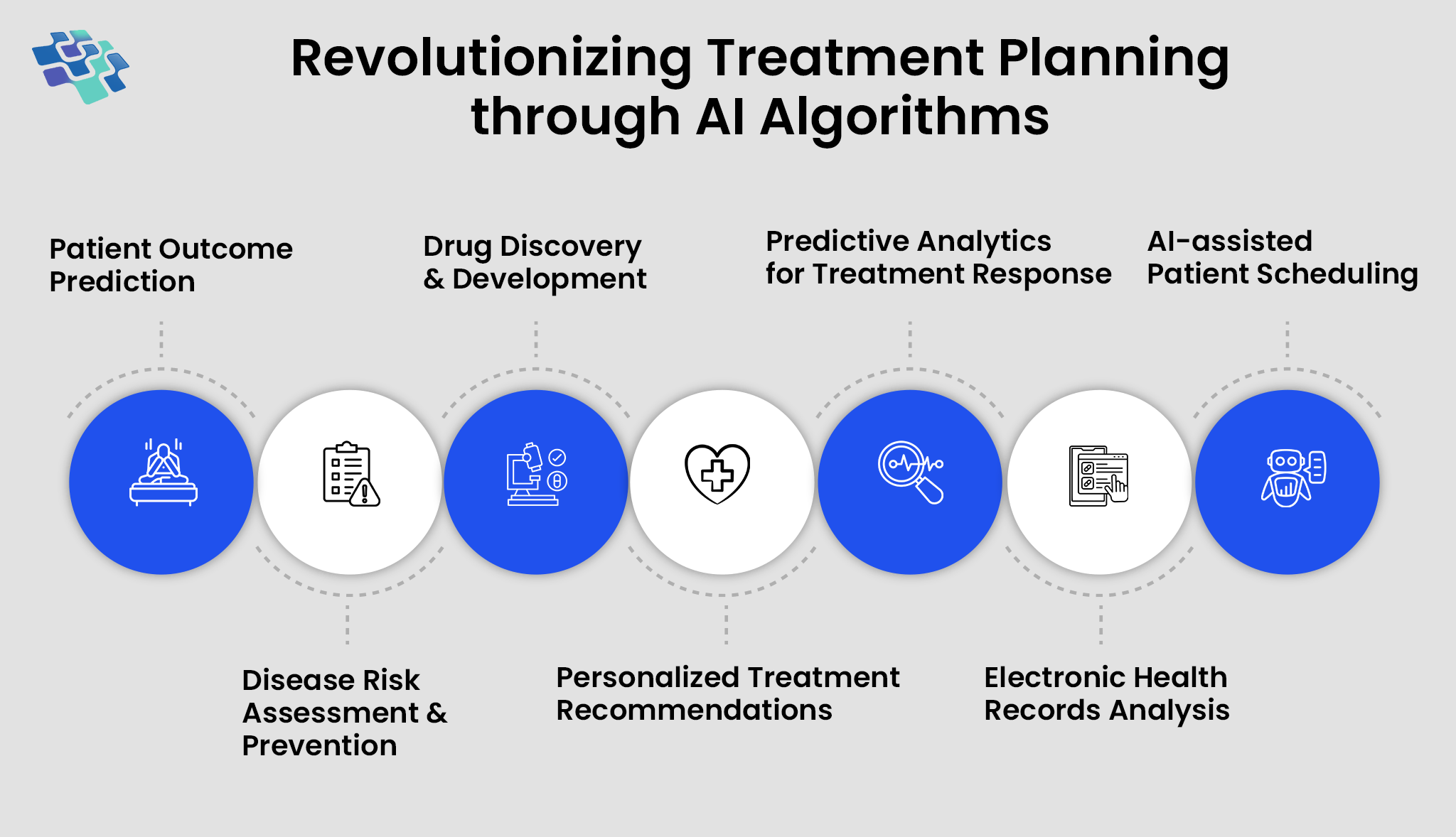
The Role of AI in Personalized Healthcare
What the American Medical Association refers to as AI’s “augmented intelligence” role is improving healthcare through better diagnostics, tailored medication...
Stay In the Know
Get Latest updates and industry insights every month.
 1. Consolidation of Patient Information
1. Consolidation of Patient Information