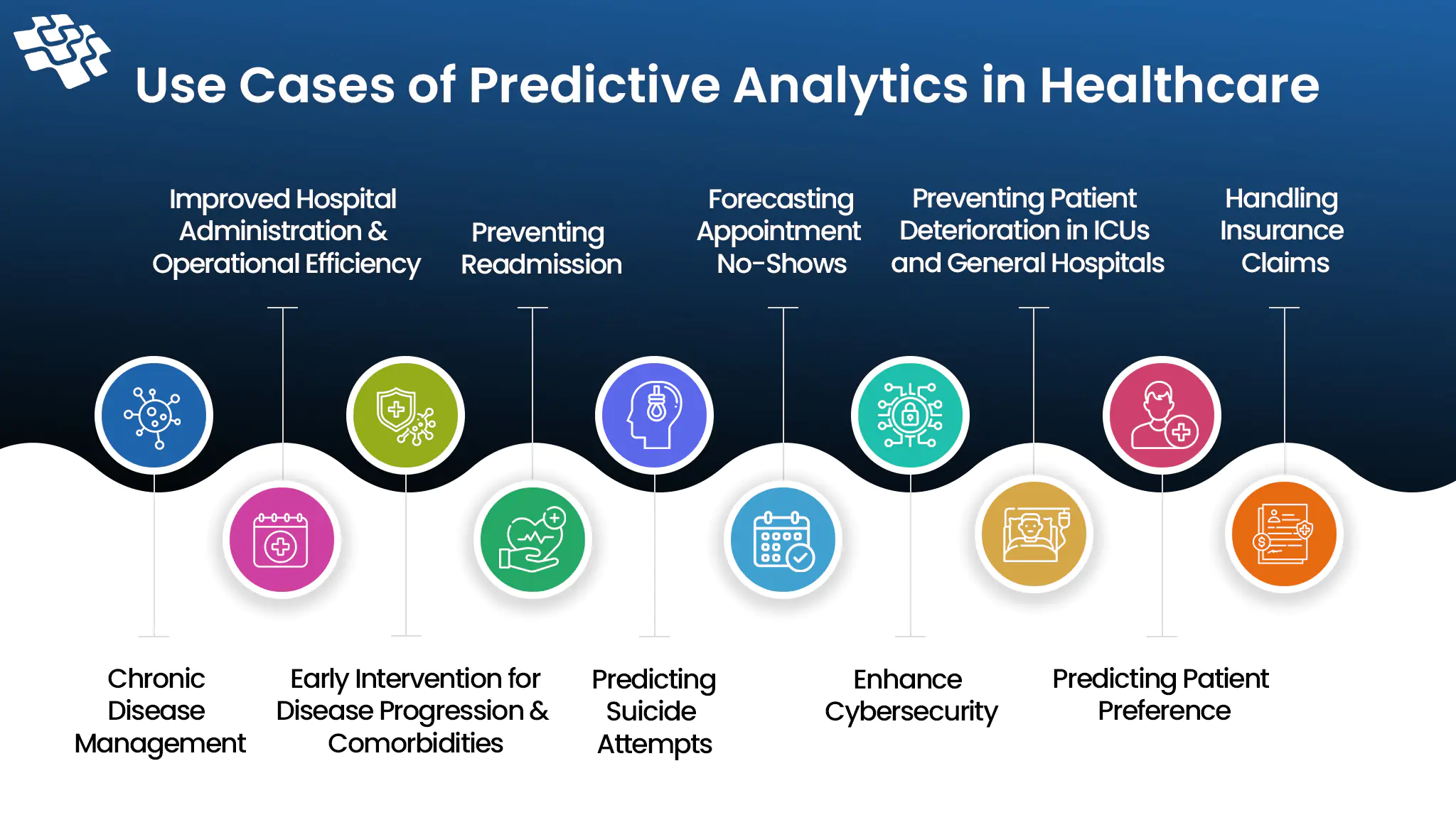
How is Predictive Analytics in Healthcare Revolutionizing It?
Imagine if medical professionals could foresee your health problems before they become critical. Predictive analytics in healthcare is real and not just science fiction.
Reduce Administrative Overhead, Eliminate Referral Leakages, and Streamline Provider-Patient Coordination with Agentic AI Automation


At NextGen Invent, we build Agentic AI-based provider operations software development services to streamline healthcare workflows, improve patient outcomes, reduce administrative costs, and enhance operational resilience. By integrating hyperautomation, predictive intelligence, and ambient AI, we transform back-office and front-office processes such as claims, referrals, policy management, and care coordination. Our services empower IPAs, ACOs, and medical groups by connecting clinical and non-clinical operations within a unified digital-first infrastructure.
We are in line with new developments in healthcare that are changing provider networks. AI-driven scheduling and credentialing are used in workforce optimization to solve staffing shortages, while ambient intelligence minimizes documentation burden to reduce clinician burden. We assist healthcare organizations in building scalable, patient-centered, and future-ready provider operations ecosystems by fusing evidence-based care models with next-generation technologies.

Standardized case bundling optimizes surgical preparation by aligning kits and case carts with 3D-planned implant lists and historical usage data. This ensures precise resource distribution, lowers disposable waste, and boosts operating room productivity. Through reducing prep variability and increasing turnover, the method promotes higher-quality surgical results, increases usage, and reduces costs.


For smooth documentation, medical supply usage events are directly integrated with EHRs and billing systems using agentic AI-enabled charge capture. Implants, consumables, and expensive disposables are automatically linked to patient information by the system, which lowers claim denials, improves billing accuracy, and speeds up reimbursement cycles. By utilizing adaptive intelligence, it reduces the amount of manual intervention, improves revenue integrity, and ensures compliance while lessening the administrative strain on providers.
Precise planning, execution, and evidence-based decision-making are made possible by advanced CAD tools and AI-driven systems, which are transforming surgical procedures. To improve early diagnosis, surgery scheduling software is excellent at interpreting medical pictures for population-wide screenings, including those for breast cancer. Cutting-edge disciplines like multiomics, which combine proteomics and genomes, use AI to generate predictive insights that aid in early diagnosis and individualized surgical treatment.


As the leading patient engagement software company, we leverage AI to transform care delivery. We identify patients for specific programs, optimize surveys, and forecast readmission risks with our cutting-edge technologies. To ensure proactive, pertinent, and outcome-driven healthcare engagements across the patient journey, conversational AI agents expedite scheduling and check-ins, sentiment analysis enhances the patient experience, and personalized engagement algorithms suggest content and follow-ups.
AI-driven revenue cycle management healthcare software optimizes RCM by automating data entry, reducing errors, and enhancing billing efficiency with Optical Character Recognition (OCR) technology. Proactive resolution is made possible by predictive analytics, which identify possible claim denials. AI automation for revenue cycle management expedites operations, reduces bottlenecks, and increases claim success rates for quicker financial results by streamlining claim routing and tracking.


AI-powered consulting and managed services improve hospital operations through resource and scheduling optimization. In addition to maximizing provider utilization and minimizing equipment downtime, intelligent algorithms also minimize patient wait times. By facilitating self-service scheduling, expediting appointment scheduling, and enabling timely follow-ups for unscheduled appointments, automated technologies enhance operational efficiency and treatment plan adherence.
Through the automation of regulatory data management and analysis, AI-powered risk and compliance software improves healthcare governance, risk management, and compliance. Data collection is streamlined, information is neatly categorized, and accurate compliance reporting is guaranteed. AI assists healthcare companies in meeting regulatory standards, enhancing quality, and fostering stakeholder and patient confidence by reducing documentation errors and streamlining audits.

Experienced AI data scientists lead seamless, customized software development with cutting-edge technologies for high-quality applications.
Deep expertise with EPIC, Cerner, Meditech, and Athena enables seamless EHR integration—backed by 500+ successfully implemented AI projects.
Proven expertise in Redox, FHIR, HL7, and 835/837 standards, including Azure and AWS FHIR implementations.
We actively listen to understand business challenges and collaborate to design tailored solutions that meet our clients' needs.
Meticulously include remarkable features for superior customer experience and market performance.
In algorithmic decision-making, we ensure transparency and accountability.
With NextGen Invent, the main impact that we saw was that we were able to resolve our problems more quickly. We had several dozen bugs in our billing system, and they were able to resolve all of those very quickly and expediently for us, allowing us to devote more time to our members and less time to dealing with billing problems. I would say that NextGen Invent's work led to a 50% increase in production. When an issue arises, we found them to be very patient, very communicative, and very responsive to our needs
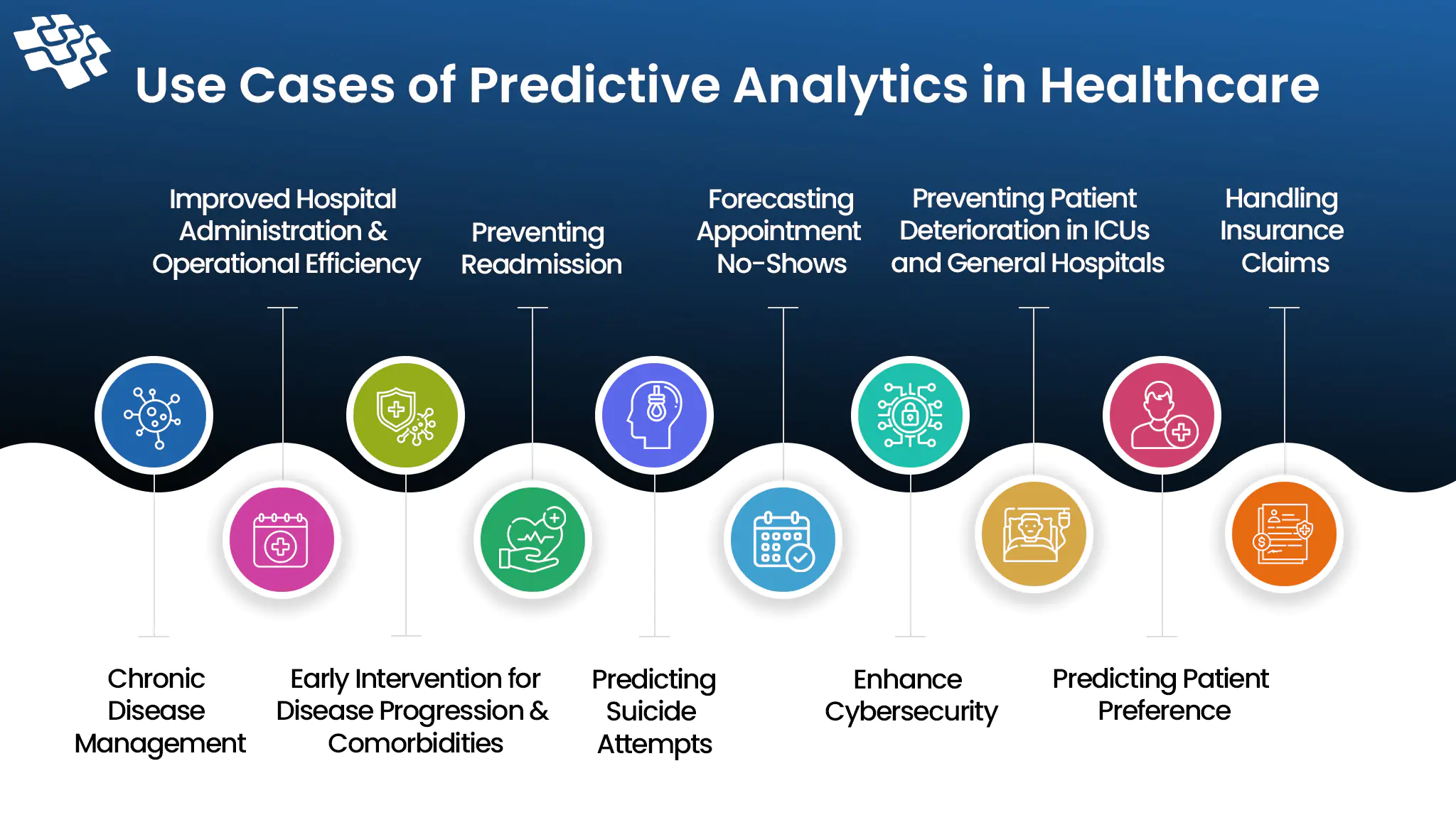
Imagine if medical professionals could foresee your health problems before they become critical. Predictive analytics in healthcare is real and not just science fiction.
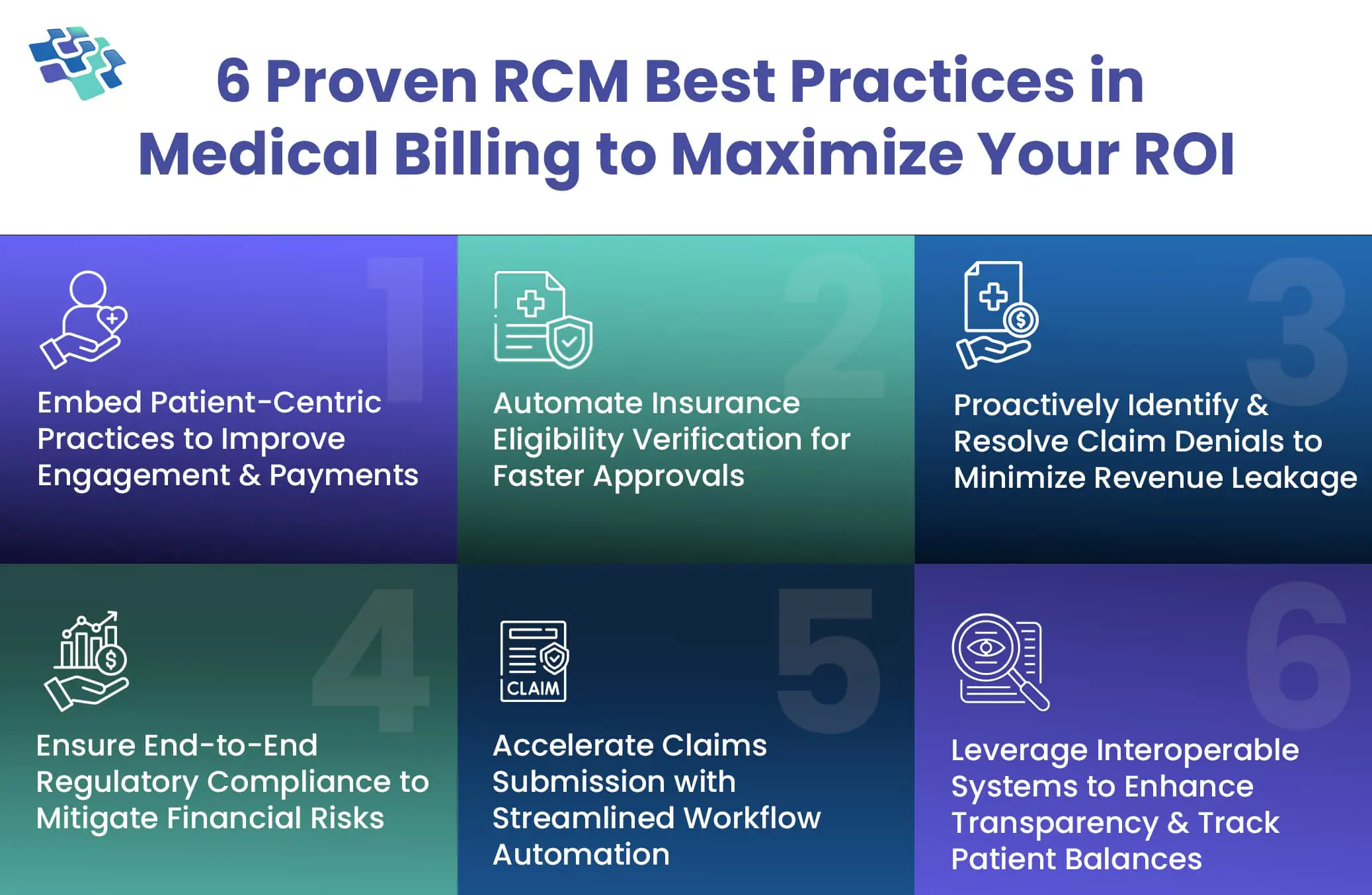
Revenue cycle management is a crucial process in healthcare that governs the financial operations, ensuring providers are accurately compensated for their services.

Healthcare is constantly evolving—and so are patient and provider expectations. Revenue cycle management systems streamline billing by centralizing financial processes for greater efficiency and accuracy.