RCM in Medical Billing: Fix Denials, Delays, and Disruptions with These 6 Proven Best Practices
For healthcare organizations, maintaining an efficient revenue cycle is key to delivering consistent, high-quality care while sustaining financial stability. By streamlining workflows and embracing digital tools, providers can minimize delays, boost revenue, and enhance patient satisfaction.
Lost In Manual Billing Errors? Improve Accuracy & Efficiency with Our Proven RCM Medical Billing Services

“According to a survey of healthcare leaders in the U.S. in 2025, the top reason for switching RCM software vendors was negative client support experiences, with almost 60% citing this reason. Another common reason for changing RCM providers was data security concerns.”– Statista
Understanding the RCM in Medical Billing
Knowing that the healthcare revenue cycle entails several clinical and administrative tasks to collect payments for patient services can help you better comprehend it. It starts with the patient’s appointment and concludes when their payment is paid. It’s a challenging but necessary process. Let’s now examine a summary of this cycle’s salient characteristics:
- Patient Registration: Getting essential information from the patient, such as basic facts and insurance information, is the first step in the revenue cycle. Getting it upfront might save you hassles when dealing with insurance, even if it may seem regular.
- Insurance Verification: Confirming what a patient’s insurance covers for their impending services is the next step, so get your Sherlock Holmes on. Knowing this ensures that the provider is aware of the amount that the insurance company will pay.
- Claim Submission: It’s time to send after you’ve arranged all of your charges nicely! They will be sent electronically to the patient’s insurance provider.
- Payment Posting: This is where the topic of money comes up. Payment (or a thorough explanation if they’re having trouble) is sent once the insurance company processes the claim. The patient’s account must appropriately reflect this payment.
So, what is the role of an RCM system? An effective RCM system minimizes delays and maximizes revenue collection by ensuring a seamless transition across the processes we just described.
How RCM Medical Billing & RCM Healthcare Services Should Reduce Administrative Costs
It’s no surprise that the U.S. healthcare industry spends over $812 billion annually on administrative costs when internal workflows routinely involve:
- Securing prior authorizations and verifying insurance eligibility
- Estimating patient financial responsibility after insurance adjustments
- Displaying accurate copayments at the point of care
- Submitting claims for maximum reimbursement
- Managing and proactively preventing claim denials
- Generating patient statements and handling related inquiries
The healthcare industry in the United States already saves $122 billion annually by automating administrative procedures. However, there is still an opportunity to save more. The US healthcare system could save an extra $16.3 billion annually if all transactions were handled electronically. That represents 42% of the industry’s current annual transaction processing expenditure of $39 billion.
Ensuring prompt and correct payment to healthcare providers for their services, whether from patient payments or other payers like health plans, is one of the objectives of revenue cycle management.
According to industry estimates, most medical offices only collect 60% of their accounts receivable, meaning they are losing out on up to 40% of their potential earnings. To optimize your revenue stream, medical billing should streamline the entire reimbursement process.
Before filing claims, the most advanced medical billing organizations employ artificial intelligence systems to detect and address issues. When payers submit appeals, resubmit denied claims, or seek further information, this helps to cut down on delays.
Building Blocks of a Revenue Cycle
The primary goal of revenue cycle management is to make sure that healthcare providers receive full payment or reimbursement for the services they render to patients. To promote better care, happier patients, engaged staff, and financial stability, the genuine return on investment goes much beyond simple billing, claims, and payment collections. The revenue cycle process is based on this benefit and is based on three needs:
- Efficiency – Reducing unnecessary resource use by streamlining procedures across the billing cycle.
- Accuracy – Lowering the number of claims denied and payment delays through early insurance coverage verification.
- Transparency – Providing prompt payment information to patients and providers will help them make educated decisions at every stage of the transaction.
Providers are moving from sluggish, expensive manual methods to digital RCM tools, which are genuinely beneficial to attain revenue cycle efficiency.
Revenue Cycle Management: Key to Successful Medical Billing
Financial sustainability and successful medical billing are based on effective revenue cycle management. For medical practices, RCM is crucial for the following main reasons:
- Improved Cash Flow: RCM in medical billing ensures correct and timely claim submission, which speeds up payments. Medical practices can satisfy their financial obligations on time since this simplifies their cash flow.
- Reduced Billing Errors: Healthcare businesses can reduce errors in coding, documentation, and claim submission by putting strong RCM procedures in place. This lowers the possibility of delays, claim denials, and income loss.
- Enhanced Patient Satisfaction: By minimizing billing-related problems, ensuring accurate and transparent billing, and promptly resolving payment-related inquiries, a seamless RCM process enhances the patient’s experience.
Struggling With Claim Denials? Discover How Our RCM Solutions Ensure Higher Accuracy & Faster Reimbursements
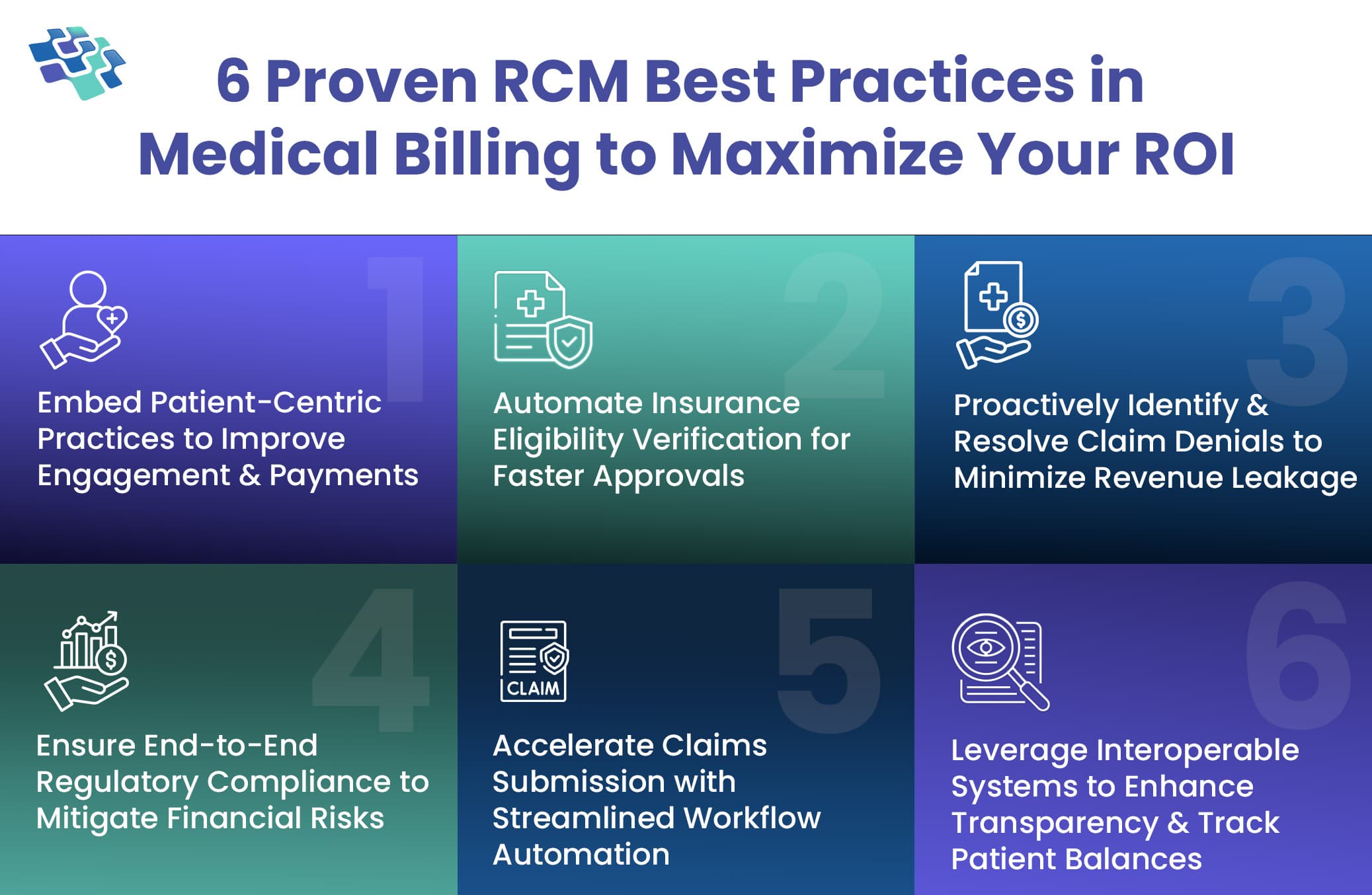
6 Game-Changing RCM in Medical Billing Tactics to Enhance ROI
Whether for integrated or virtual treatment, doctors are gradually embracing healthcare automation techniques. Healthcare professionals need to use RCM healthcare services to increase their capital. To assist you in achieving high returns on investment, we have compiled a list of the top 6 practices for healthcare revenue cycle management.
 1. Embed Patient-Centric Practices to Improve Engagement & Payments
1. Embed Patient-Centric Practices to Improve Engagement & Payments
To increase their revenue and enhance healthcare administration, medical practices must use RCM medical billing services. The staff should take the initiative to boost patient participation to promote trust and enhance patient outcomes. Healthcare providers must use revenue cycle management to explain to patients, both orally and in writing, their financial obligation, available payment methods, and what to expect from their visit.
Patients should be the primary focus of a doctor’s time and energy, not the pursuit of greater financial gain. The revenue cycle management process in medical billing may be perceived by patients as difficult, perplexing, and confusing. With custom AI mhealth app development, healthcare providers may allay these issues and motivate patients to embrace online billing and payment.
2. Automate Insurance Eligibility Verification for Faster Approvals
When incorporating RCM into medical practice, confirming insurance coverage at the time of patient registration is a crucial step. An increasing number of insurance providers set strict guidelines for eligibility for coverage and prior authorization software with revenue cycle management.
Using medical revenue cycle management to automate insurance verification can streamline clinical procedures, expedite payment reimbursement, and lessen administrative staff effort. Denials of claims can also be prevented by using RCM in medical billing to automate insurance verification.
3. Proactively Identify & Resolve Claim Denials to Minimize Revenue Leakage
Many medical billing management practices do not have an RCM because of claim denials. There are several reasons why claims may be denied, including coding errors, duplicate claims, incomplete information, missing deadlines for filing claims, and more. For this reason, it is crucial to keep a close eye on the claim procedure. RCM solutions can assist you in comprehending each claim and determining the reasons behind claim denials.
In medical billing, RCM can help your employees spot trends and errors so you can avoid denials of claims. It can help you better manage claim denials by keeping track of denials and the reasons behind them. To reduce the likelihood of denials, a medical billing denials prevention program should be put in place that focuses on standardizing procedures for all employees.
4. Ensure End-to-End Regulatory Compliance to Mitigate Financial Risks
When offering healthcare services, whether virtually or in person, healthcare systems are required to abide by all compliance rules, including HIPAA. To manage the RCM in medical billing, HIPAA regulations mandate that all healthcare providers submit claims electronically in an approved way. Record-keeping paperwork can result in errors and not meet HIPAA’s requirements for accuracy.
Healthcare professionals can protect patient privacy, security, and confidentiality by adhering to HIPAA regulations. Our RCM healthcare services at NextGen Invent encourage both correct medical record filing and HIPAA compliance.
5. Accelerate Claims Submission with Streamlined Workflow Automation
Healthcare workers frequently make the mistake of missing deadlines and not filing claims on time. The period from the date of healthcare service to the filing of a claim ranges from three months to a year, depending on the payor. Revenue loss occurs if the claim is not submitted within the allotted period.
Under such conditions, the medical staff would not be able to receive payment for their clinical work. Because we understand that you don’t want this to occur, RCM healthcare services make sure that the claims are submitted within the allotted time.
Check our case study on: Affordable Health Plan, and Insurance Claims Processing
6. Leverage Interoperable Systems to Enhance Transparency & Track Patient Balances
One of the essential features of RCM software is interoperability. It ensures that patient data is securely transferred between the many healthcare networks that provide patient care. RCM solutions that are interoperable encourage collaboration and simplify processes for a range of healthcare providers.
Interoperable medical billing solutions simplify billing administration and uphold HIPAA compliance by providing healthcare analytics and electronic data exchange across multiple systems and devices.
Tired of Payment Delays? Streamline Your Cash Flow with Our End-To-End RCM in Medical Billing Software Development Services
What Areas of the RCM Process Can Benefit from Agentic AI?
- Claims Status: Agentic AI can automate the process of checking and updating claims status across multiple payers, reducing manual effort, minimizing errors, and accelerating reimbursements by proactively resolving delays and flagging discrepancies for human review.
- Eligibility Prior Authorization: Agentic AI can instantly verify patient eligibility and initiate prior authorization requests, navigating payer-specific requirements. It improves approval turnaround times, reduces denials, and ensures accurate data capture—enhancing patient experience and administrative efficiency.
- AR Management: Agentic AI can autonomously monitor accounts receivable, identify aging claims, prioritize follow-ups, and act based on payer responses. This improves cash flow, reduces write-offs, and ensures the timely resolution of outstanding claims with minimal human intervention.
- AI-Based Chatbot: Agentic AI-powered chatbots can handle routine patient and payer queries around billing, insurance, and claim status. They offer 24/7 assistance, reduce call center burden, and escalate complex issues intelligently, enhancing operational efficiency and patient satisfaction. Check our case study on: Voice Enabled, AI Powered Healthcare Chatbot
Change How You Approach RCM in Medical Billing by Partnering with NextGen Invent
Efficient RCM in medical billing is critical to healthcare providers’ financial stability. There are several benefits to RCM, ranging from lowering claim denials to ensuring patient happiness. Through comprehension of every phase, surmounting typical challenges, and utilizing technology, providers can enhance their RCM procedures, leading to a more seamless billing process, more robust cash flow, and enhanced operational effectiveness.
At NextGen Invent, our AI healthcare mobile app development services combine advanced claims processing with tailored performance consulting to deliver a smarter, more strategic approach to revenue optimization. Whether you’re a small physician group or a large hospital system, we offer end-to-end support that goes far beyond routine reporting and automation.
Our approach consistently delivers measurable results, including an ensured 12% increase in cash flow and a reduction in accounts receivable days to under 40. Driven by an entrepreneurial mindset, deep industry expertise, and a relentless focus on client success, we empower healthcare providers to streamline operations and unlock long-term value.
Reach out today to discover how our services can work for you.
Frequently Asked Questions About RCM in Medical Billing
Related Blogs
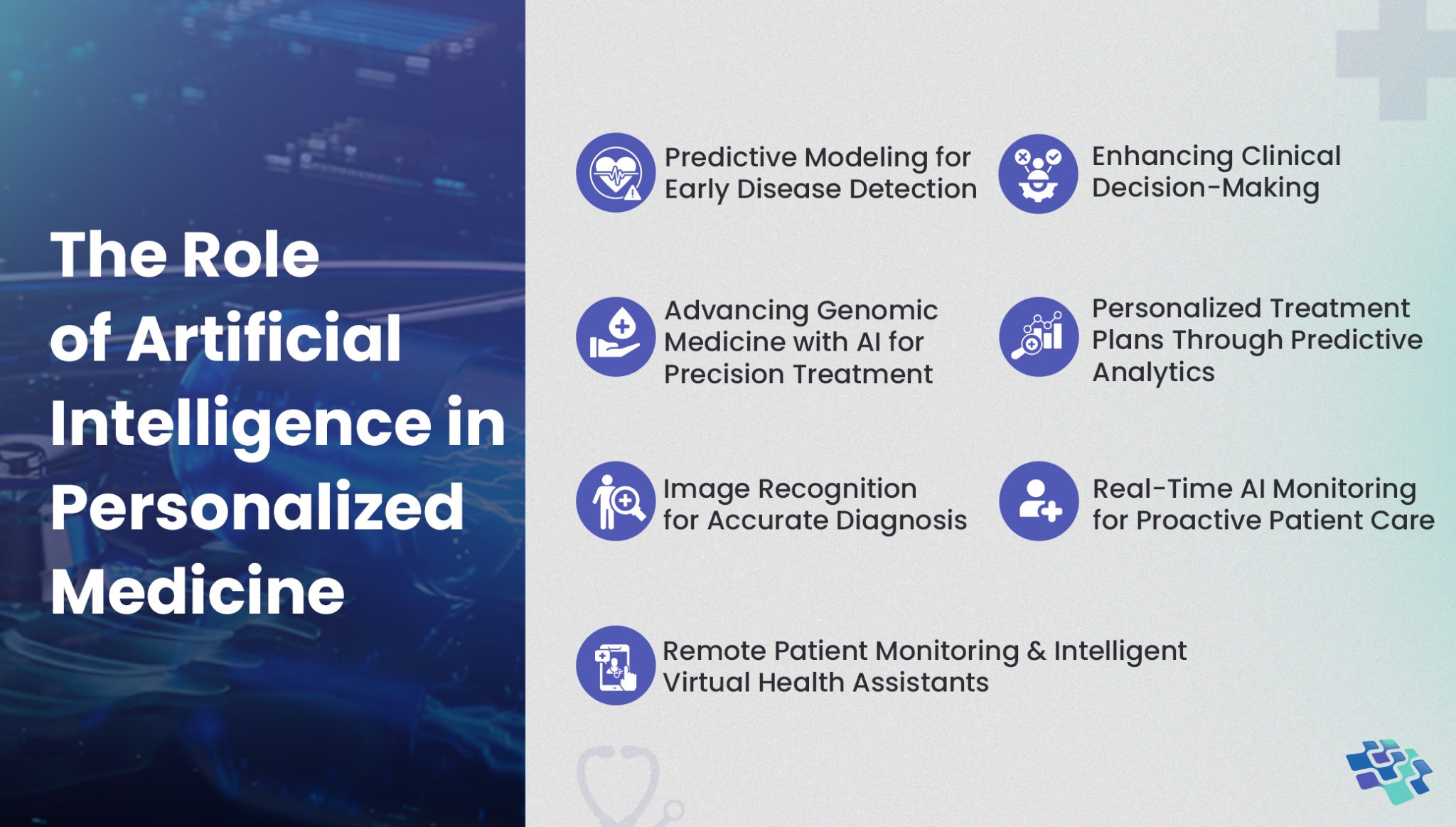
AI in Personalized Medicine: Solving Delayed Diagnoses for Better Patient Outcomes
The rapid growth of new medications, treatment protocols, and evolving regulations is outpacing healthcare providers’ ability to stay updated. AI in personalized medicine helps bridge this gap, enabling timely decisions by analyzing vast data and delivering actionable insights in real-time.
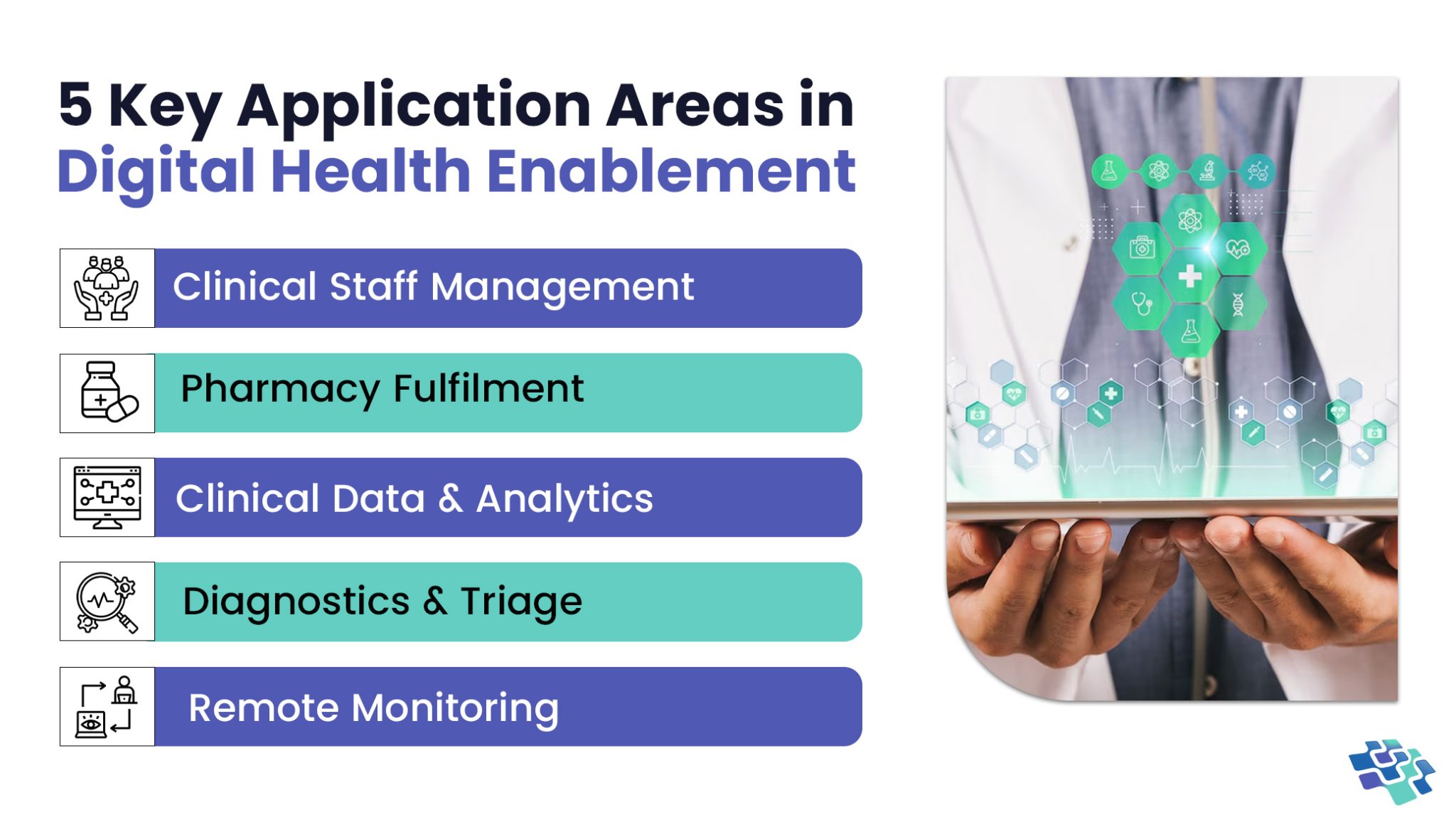
Unlocking Healthcare Innovation through Digital Health Enablement
What defines an effective digital health enablement system? Having quick and easy access to the data you need is undoubtedly important. A few minutes of delay in accessing data could mean the difference between life and death in healthcare delivery organizations where every second matters.
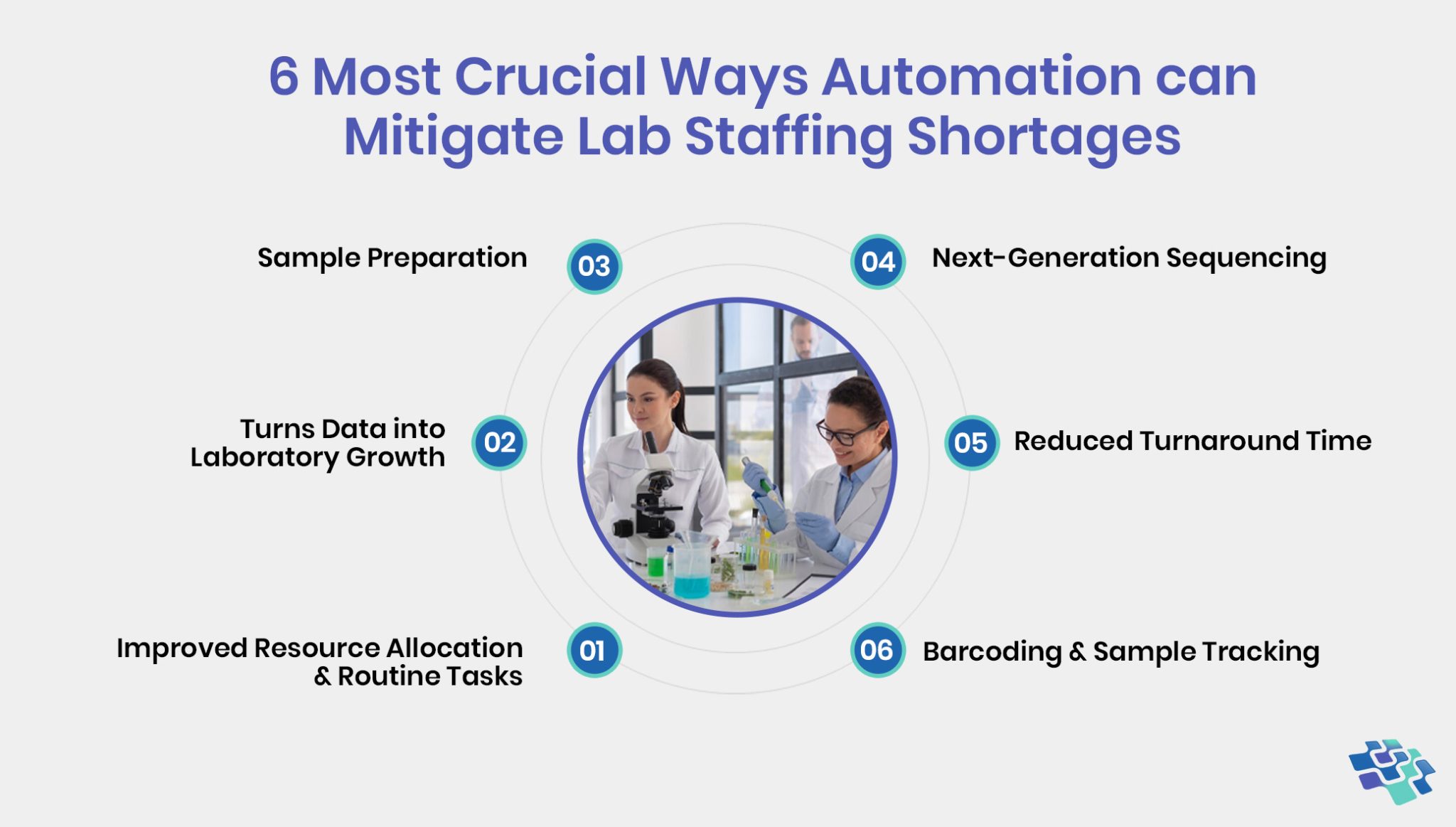
Struggling with Staffing Shortages? Discover How Lab Automation Can Solve the Crisis!
The lack of lab personnel has been an issue for many years and has now reached a critical stage. An estimated 20,000 to 25,000 laboratory technologists are needed nationwide, with vacancy rates as high as 25% in some US regions.
Stay In the Know
Get Latest updates and industry insights every month.
 1. Embed Patient-Centric Practices to Improve Engagement & Payments
1. Embed Patient-Centric Practices to Improve Engagement & Payments