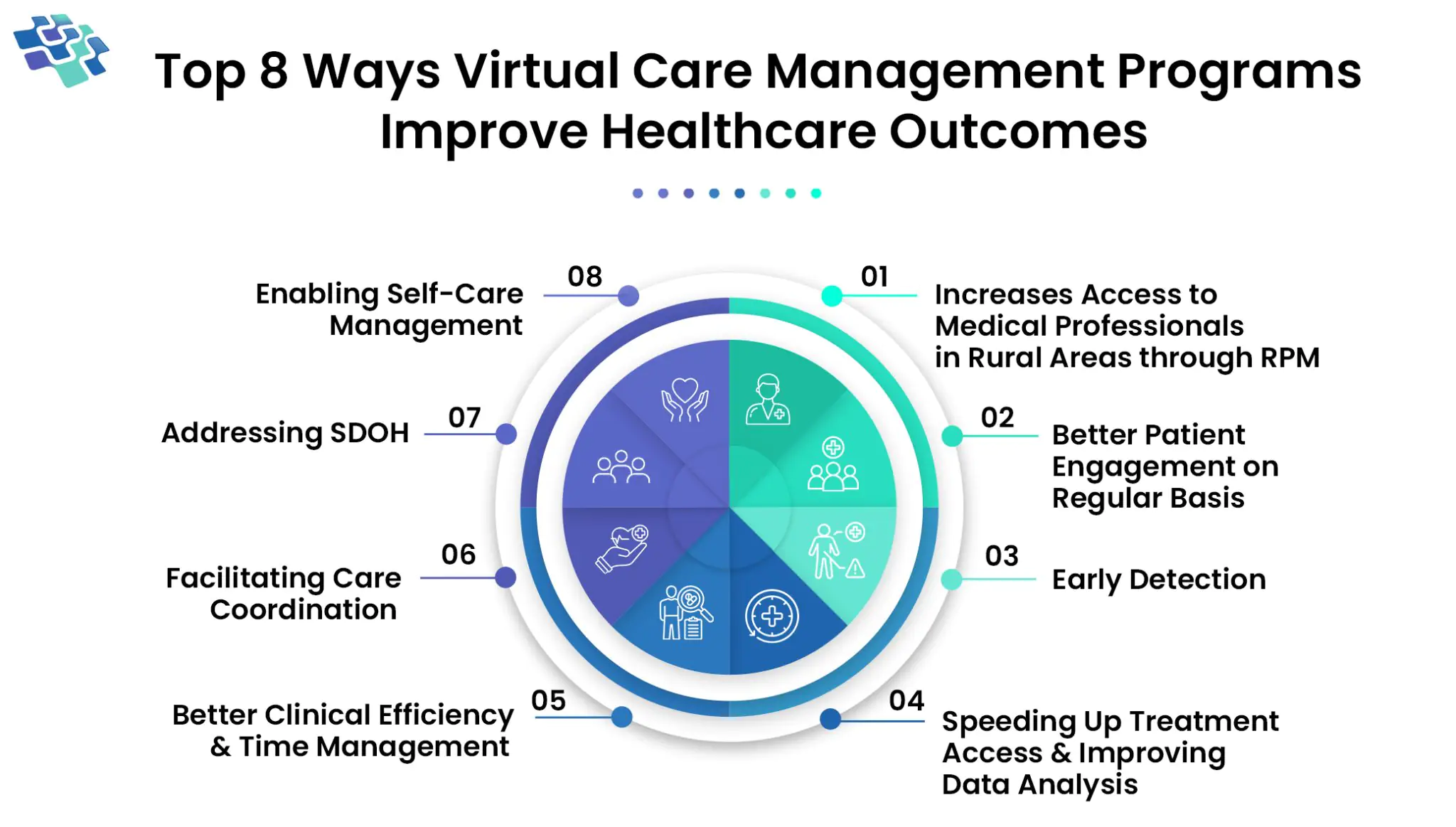
How Virtual Care Management Programs Improve Patient Wellness
Are you curious about the future of virtual health and what it entails?

Enabling Payer-Provider Collaboration with Outcome-Driven Strategies

At NextGen Invent, we provide AI-powered managed care software services to optimize case administration, enrollment, authorizations, billing, payments, and reporting, among other healthcare activities. Throughout the healthcare ecosystem, our solutions increase care quality, streamline workflows, reduce administrative burden, and improve coordination by utilizing predictive analytics, adaptive AI models, and autonomous decision intelligence.
We enable healthcare organizations to:
We enable IPAs, PBMs, TPAs, payers, and managed care organizations to use Agentic AI, composite AI systems, and real-time interoperability frameworks. Our services and solutions enhance practice management software to improve care delivery, cut costs, and produces quantifiable gains in patient outcomes and operational efficiency.

AI-driven care coordination integrates real-time data sharing between care teams to ensure smooth patient care management. By aligning care delivery with patients’ needs and preferences, artificial intelligence enhances communication, automates care pathways, and optimizes clinical decision-making, delivering high-quality, personalized, and cost-effective healthcare outcomes.


AI-powered cost containment in managed care optimizes resource allocation by identifying inefficiencies, automating claims processing, and predicting spending trends. AI uses predictive analytics and real-time data insights to save unnecessary spending. This improves affordability, increases access to preventive treatment, and benefits patients, healthcare systems, and providers.
AI in Payer Operations optimizes claims processing, fraud detection, and care management through machine learning and natural language processing. Advanced healthcare analytics and workflow automation enhance operational efficiency, reduce costs, and improve patient outcomes. AI-driven insights streamline member engagement and provider network management for superior payer performance.


AI-powered medication management improves adherence by analyzing drug-drug interactions (DDIs) and predicting individual medication responses. Machine learning algorithms personalize treatment plans, optimizing therapeutic outcomes and reducing adverse drug events. This leads to enhanced medication safety, reduced total cost of care, and improved health outcomes across patient populations.
AI enhances provider network optimization by leveraging predictive analytics to assess provider performance, patient outcomes, and cost efficiency. By identifying high-value providers and employing contract negotiation algorithms, payers can improve care quality and reduce costs, ensuring better value-based care delivery for members and optimizing network performance.


AI-driven risk and quality management in healthcare enhances fraud detection by analyzing claims data for anomalies such as duplicate claims or abnormal billing patterns. Using machine learning algorithms, these systems continuously evolve, improving accuracy and efficiency over time, enabling payers to proactively manage financial risks and improve care quality.
AI-driven self-directed care empowers users to monitor physical activity, track nutrition, and receive personalized wellness plans. AI chatbots analyze user data for early detection of health risks and emotional disturbances, enabling preventive care. Virtual assistants enhance engagement, streamline inquiries, and optimize appointment scheduling, improving efficiency and reducing healthcare burden


AI enhances TPA operations by automating claim processing, leveraging machine learning models to analyze data and detect fraud patterns. AI-driven insights optimize policy administration, streamline customer interactions, and improve operational workflows. By reducing manual tasks and improving predictive analytics, AI boosts efficiency and delivers superior service for insurers and policyholders.
Automated workflows improve claims accuracy, cut down on delays, and eliminate manual approvals. Managed care software improves patient satisfaction and payer-provider operational efficiency by expediting the prior authorization and claims review processes, lowering administrative burden, and ensuring timely treatment delivery.
Reminders, notifications, and personalized digital interactions promote compliance with wellness initiatives, preventive screenings, and care plans. Managed care software increases long-term loyalty to the health plan, lowers preventable complications, and improves health outcomes by actively engaging with the members.
Chronic diseases, high-risk members, and usage trends are identified using advanced predictive analytics. Managed care platforms enhance population health outcomes and optimize resource allocation across a number of patient populations by facilitating proactive interventions, tailored care programs, and preventative measures.
AI-powered, personalized engagement solutions reduce administrative procedures, increase communication, and expedite encounters. Faster approvals, precise billing, and proactive care suggestions increase member happiness and loyalty, lower attrition, and increase retention and long-term trust in the managed care organization or health plan.
Advanced formulary management and predictive cost analytics minimize unnecessary expenditures, reduce medication waste, and prevent cost overruns. Managed care software identifies high-cost therapies, enables formulary adherence, and delivering measurable savings while maintaining quality and effectiveness of patient treatments.
Experienced AI data scientists lead seamless, customized software development with cutting-edge technologies for high-quality applications.
Deep expertise with EPIC, Cerner, Meditech, and Athena enables seamless EHR integration—backed by 500+ successfully implemented AI projects.
Proven expertise in Redox, FHIR, HL7, and 835/837 standards, including Azure and AWS FHIR implementations.
We actively listen to understand business challenges and collaborate to design tailored solutions that meet our clients' needs.
Meticulously include remarkable features for superior customer experience and market performance.
In algorithmic decision-making, we ensure transparency and accountability.
NextGen Invent's comprehensive data science services, including classifier development and knowledge graphs, bolstered healthcare innovation. Their mass spectrometry algorithm showcased machine learning and software engineering prowess.
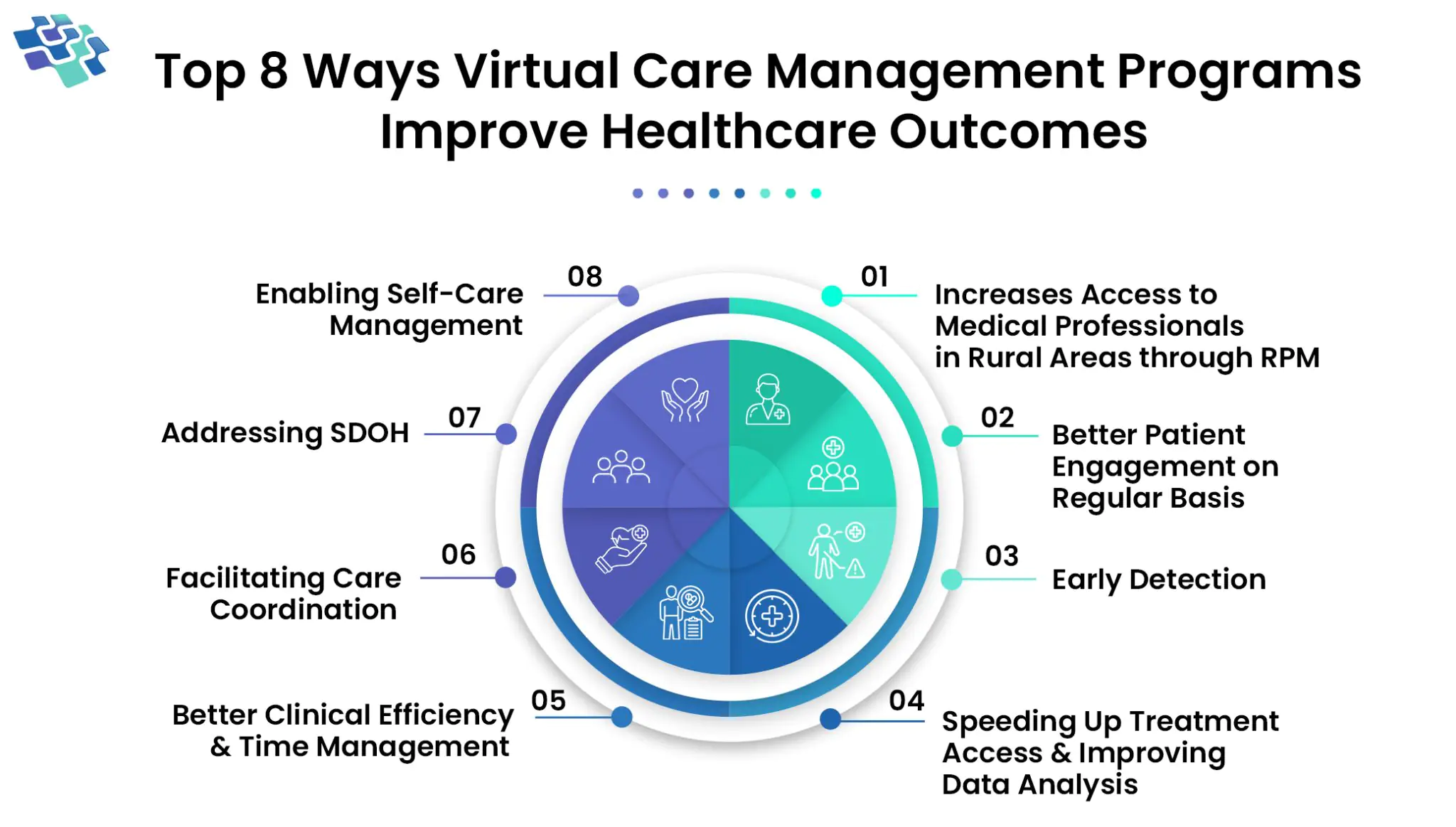
Are you curious about the future of virtual health and what it entails?
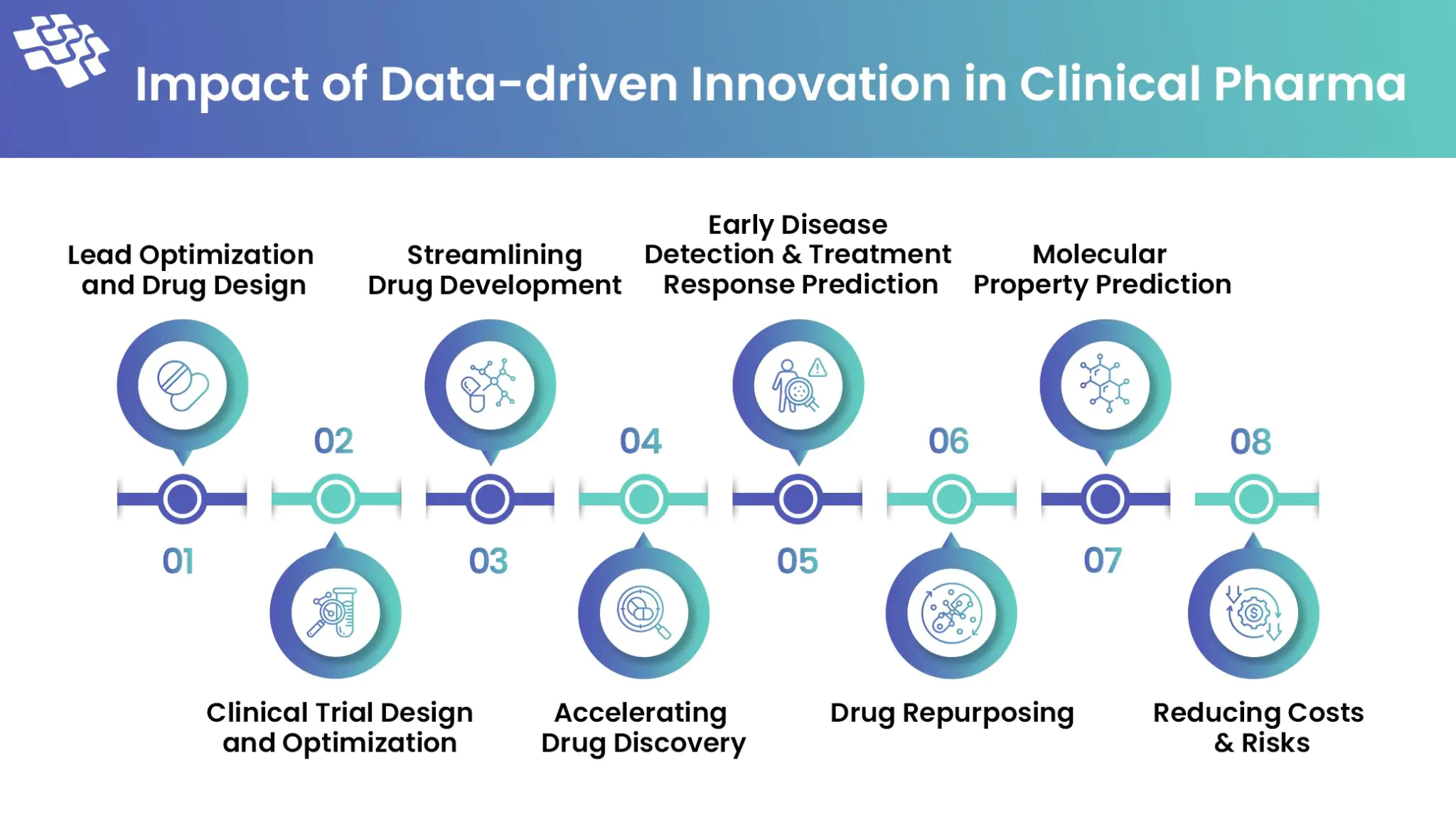
The critical significance that machine learning and big data play in speeding up drug development and discovery will be discussed in this article.
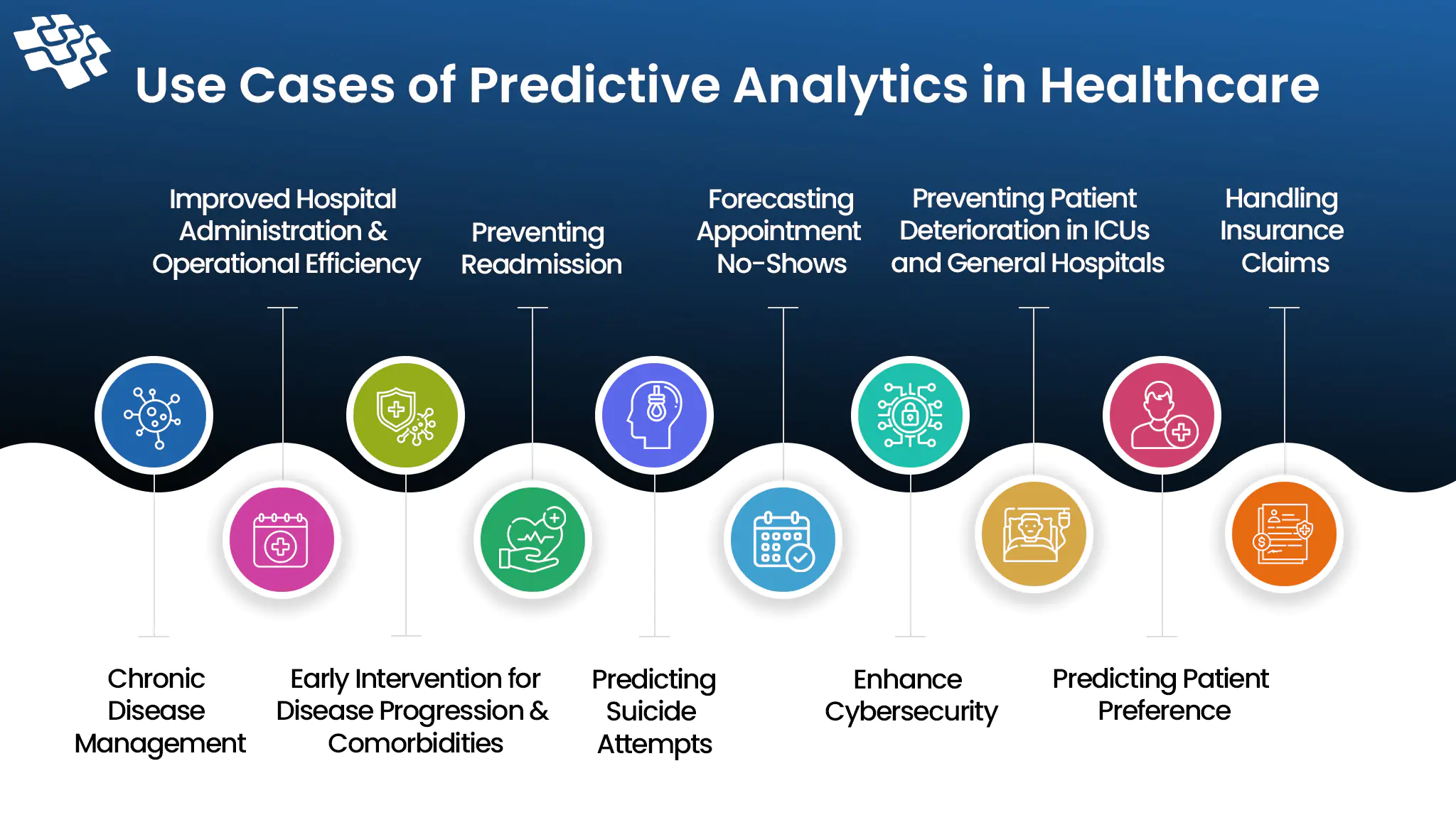
What if your health issues could be predicted by medical specialists before they become serious? Check how predictive analytics is doing that.