Unlocking Revenue Growth: The RCM Process Flowchart That Solves Claim Denials & Payment Delays
By centralizing operations under a single call center roof, they can assist clinics operate more efficiently on their end and improve patient service during difficult financial times.
Overwhelmed By Administrative Work? Automate Tedious Tasks with Our Smart RCM Healthcare Technology

“The revenue cycle management (RCM) market size is expected to grow rapidly in the next few years. It will grow to $275.86 billion in 2029 at a CAGR of 15.2%. The growth in the forecast period can be attributed to the transition to value-based care models, integration of AI and machine learning in RCM, telehealth, and remote patient interactions, patient-centric financial experiences, consolidation of RCM services, addressing billing and coding complexities, enhanced data analytics for revenue optimization.”– The Business Research Company
Understanding Healthcare RCM Process Flowchart
The financial journey of a patient’s interaction with a healthcare provider can be represented by the healthcare RCM cycle flow chart. It describes the detailed procedures for billing, coding, filing claims, and reimbursement, starting with registration and ending with final payment.
Fundamentally, the RCM process flowchart helps healthcare organizations in understanding and streamlining their revenue cycle processes. Stakeholders can use it to find bottlenecks, inefficiencies, and areas for change. By providing a clear and organized perspective of the revenue cycle, the RCM flowchart improves overall efficiency, minimizes errors, and simplifies financial procedures.
Every stage of the revenue cycle is interrelated, and a well-designed RCM process flowchart makes it easier to see how these stages depend on one another. It gives employees the authority to adhere to established protocols, resulting in reliable, error-free processes. Additionally, the RCM flowchart encourages increased departmental collaboration and communication, which eventually boosts income production and the healthcare organization’s financial stability.
To maximize revenue and ensure the financial stability of healthcare providers, it is essential to comprehend and use the healthcare RCM cycle flow chart.
Importance of RCM Process Flowchart
- Standardizes processes for consistency across the revenue cycle.
- Identifies key revenue drivers to support strategic planning.
- Enhances order processing, improving customer satisfaction.
- Streamlines patient billing in healthcare through clear workflow mapping.
- Enables data-driven decisions through visualized process data.
- Clarifies task ownership by defining individual roles.
What is RCM Workflow?
To optimize their financial operations, healthcare providers must have a solid understanding of the RCM workflow. By asking what RCM workflow is, one can have a thorough understanding of the sequence of steps and processes that go into handling the financial facets of patient care, from the first patient engagement to the last payment collection. In healthcare organizations, it is essential to preserve both financial stability and effectiveness.
- Initial Patient Interaction: This important initial phase is obtaining and confirming patient data, laying the groundwork for all ensuing financial transactions.
- Medical Billing Process Steps: This involves converting the recorded services into uniform billing codes, a procedure that calls for close attention to detail.
- Claims Submission: A crucial stage in the revenue cycle is reached when claims are produced and sent to insurance companies following coding. Check Our Case Study: Affordable Health Plan and Insurance Claims Processing
When it comes to the medical billing procedure, accuracy is crucial. Coding or documentation errors may result in claims being rejected, which can cause losses and administrative work. As a result, sustaining an efficient RCM workflow requires ongoing training and code expertise updates.
The effective management of a healthcare provider’s financial health depends on a strong RCM workflow. It is a complicated but necessary system that combines patient-centered treatment with financial stability.
How Can Hospitals Improve the RCM Cycle in Medical Billing?
Healthcare providers should adhere to best practices such as these to maintain seamless billing and revenue collection:
- Automating RCM Processes: Utilizing RCM healthcare services or software to monitor claims, confirm insurance, and minimize human error.
- Focusing on Patient Communication: Providing patients with clear billing explanations aids in their understanding of their financial obligations.
- Regular Audits: RCM health care performance checks assist in finding errors before they become significant issues.
- Training Medical Billing Staff: Accurate claims administration and coding are made possible by a skilled staff.
According to a study, claim denials decreased by 20% in hospitals that used AI-based RCM healthcare services.
Experiencing Poor Cash Flow? Partner With Us to Accelerate Collections & Improve Financial Stability
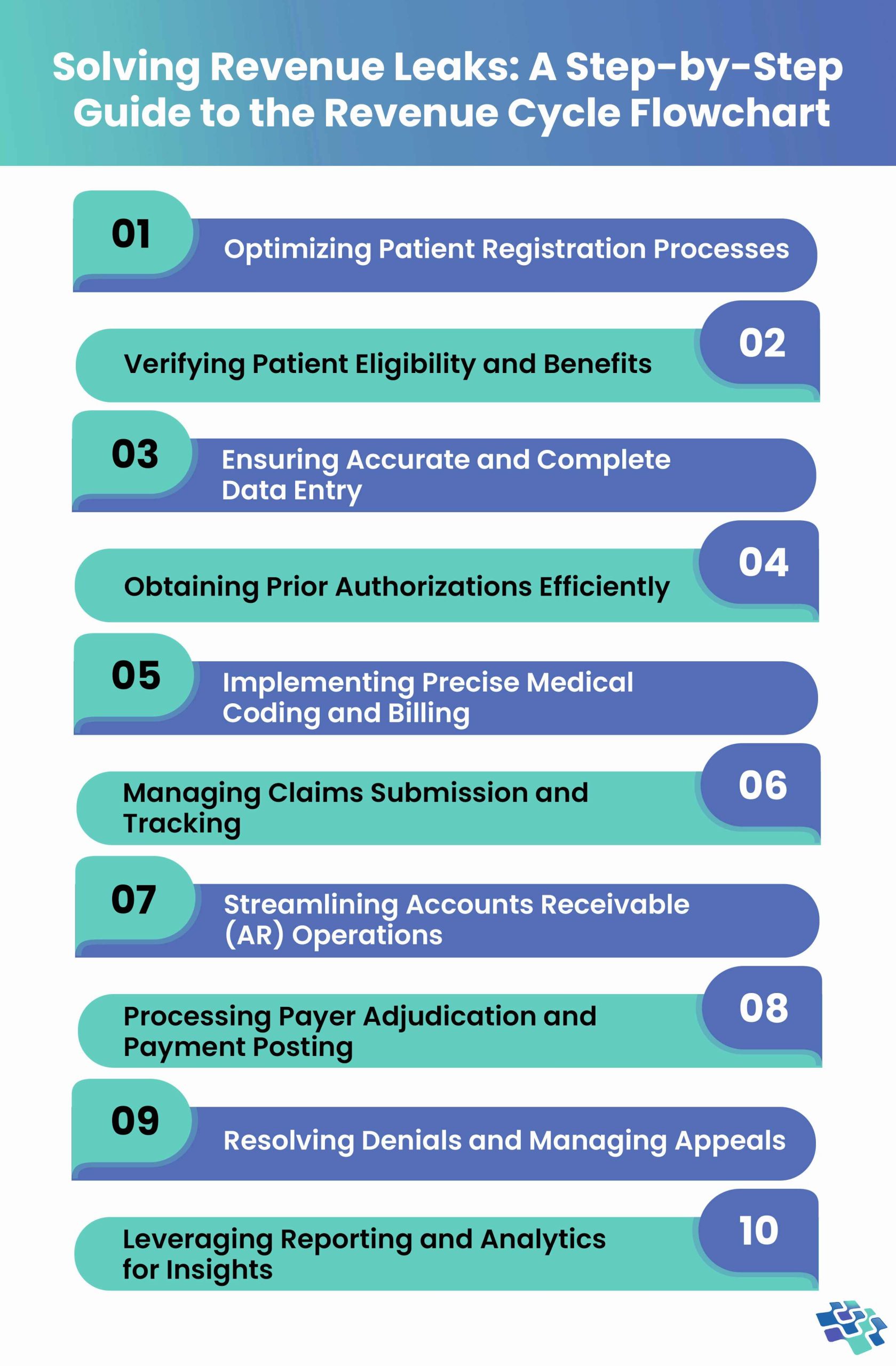
Key Stages in the RCM Process Flowchart
A thorough and reliable strategy that effectively manages all the essential tasks, from patient registration to coding and payment collection, is the secret to a successful RCM process flowchart.
 1. Optimizing Patient Registration Processes
1. Optimizing Patient Registration Processes
Getting patients registered is the first step to an effective RCM process flowchart. Consequently, the procedure ought to be as quick and easy as feasible. By using patient portals and practice management software, operational and clinical productivity can be increased. In this step, patient data needed for medical records is collected. This includes contact information, diagnosis, current medication, past medical history, and general demographics. Future care services for the patient depend on this information.
Leading RCM businesses surpass the conventional cost and bottom-line growth targets by utilizing creative tactics. To employ practice management software and reduce billing expenses, RCM healthcare services uses all the innovative techniques and ideas.
2. Verifying Patient Eligibility & Benefits
One of the most crucial phases in the RCM process flowchart is eligibility verification. The insurance company is an external party involved in this procedure. To find out how much the insurance company will pay for the treatment rendered, it is necessary to verify the patient’s insurance eligibility. This would enable the physician to disclose any co-pays up front to the patient. To improve the likelihood of consistent cash flow and prevent denials, it is advised to verify the patient’s insurance coverage, eligibility, and benefits. If eligibility is not verified beforehand, the provider may lose money. For instance, the patient cannot afford the treatment if the payer fails to verify that the services are rendered. The costs will be covered by the provider.
Therefore, the long-term financial stability of your business requires ensuring eligibility verification before offering services. Policy carrier, policy status, plan type, age covered, co-pay data, family information, pre-authorization, claim submission, and more are all included in medical verification. Before providing ai healthcare mobile app development services, medical practices must use Electronic Health Records software to confirm patients’ eligibility and benefits.
3. Ensuring Accurate & Complete Data Entry
Precise data entry comes before proper claims filing. Due to denied claims, inaccurate data entry causes incorrect billing and coding, which eventually leads to lost income or sluggish revenue collection. Accurately submitting the data reduces billing expenses and protects you against refused claims. Denials of health insurance claims are increasing; a survey found that the denial rate is between 10% and 20%, which raises your billing expenses and decreases the effectiveness of your practice.
To verify patient IDs and link the appropriate data to the appropriate person, accurate data entry is essential. This accuracy is essential for improving proficiency and lowering medical billing errors.
4. Obtaining Prior Authorizations Efficiently
Prior authorizations must be determined by physicians before the start of therapy. In that case, they must request the payer. Without prior authorizations, providers risk having their claims rejected, which raises expenses, necessitates laborious rework, and makes patients’ experiences distressing.
Prior authorizations lead providers through a process that streamlines submissions, status checks, and questions. Using real-time data on each payer’s prior authorization requirements, which is kept in the pre-authorization knowledge base, it automatically fills in payer data. To speed up treatment and ensure on-time payments, prompts for manual involvement ensure the procedure is as effective as feasible.
5. Implementing Precise Medical Coding & Billing
Providers must verify payer codes for rendered services before initiating patient billing. To ascertain due amounts, payers utilize a variety of codes, including diagnostic (Dx), place of service (POS), current procedural terminology (CPT), and Healthcare Common Procedure Coding System (HCPCS) codes. Claims are likely to be rejected if codes are entered incorrectly.
Before a claim is submitted, automated claims management software can verify that it is accurate and complete. They include both client-specific tailored adjustments and standard worldwide edits for commercial payers and the government, allowing providers to submit claims with confidence.
6. Managing Claims Submission & Tracking
To submit clean claims, the most crucial steps are coding and documentation. Complete paperwork and accurate coding ensure that claims are processed accurately, paid out on time, and appropriately. Any dental professional will tell you that it has become increasingly difficult to submit claims that are reimbursed the first time. The area of your revenue cycle management process that benefits the most from having RCM specialists on your team is insurance revenue. RCM specialists are masters in figuring out how to reduce expenses, reverse denials, and obtain quicker reimbursements.
Policies, rules, and codes are subject to constant change. In the absence of committed professionals to maintain the process current and compliant, hundreds or even millions of dollars are not collected.
7. Streamlining Accounts Receivable (AR) Operations
In AR management, unpaid claims are pursued until they are settled. It entails keeping an eye on and handling pending claims to make sure they are revised, settled, and denied appeals until they are paid and posted. The insurance providers are held responsible for adhering to the conditions of your contract by AR management. AR management at a prominent level will result in better cash flow and fewer write-offs. This is because there is no money left on the table or in the bank’s possession. An expert is attempting to follow up on outstanding insurance claims and appeal denials to make sure you receive the money you are due.
A/R management will:
- Accelerate revenue collection
- Minimize overwhelming debt
- Enhance regulatory compliance
- Boost patient satisfaction by optimizing benefit utilization
RCM specialists will be aware of the most effective methods and techniques for interacting with insurance providers and contesting denials until your claims are settled.
8. Processing Payer Adjudication & Payment Posting
The process by which payers examine submitted claims and decide whether to repay them is termed as payer adjudication. Based on coverage, medical necessity, and policy provisions, the claims’ validity is assessed during this step. Payments are deposited into the patient’s account following the adjudication of the claims. When payments are posted accurately, the account balance and, if relevant, the patient’s future billing are reflected. Furthermore, effective phase management ensures that healthcare providers can precisely track their revenue, spot any irregularities, and ensure that all treatments are paid for.
Healthcare providers can employ automated payment posting systems that work with their billing software to make this procedure easier. These technologies can reduce the amount of manual labor needed to reduce errors and match payments to related claims in a timely and correct manner. Accurate recording of received funds is also made possible by routinely reconciling bank deposits with payment postings. This stage also offers the chance to find any discrepancies or underpayments that would need to be followed up with the payers.
9. Resolving Denials & Managing Appeals
Although denials are an unavoidable aspect of the healthcare revenue cycle, their effects can be lessened through effective denial management. Resubmitting claims with corrections, addressing the underlying issues, and determining the reasons for denials are all steps in this procedure. Healthcare providers can also challenge denials through the appeals process as necessary to avoid losing out on revenue. Maximizing revenue and preserving financial stability require a denial management plan. Healthcare providers can lower the number of refused claims and increase their total collection rates by proactively managing denials.
This procedure can be made more efficient by putting in place a denial management system. Billing personnel can swiftly prioritize and resolve the most frequent problems by gathering denial information from the clearinghouse, such as the denial reason. Frequent analysis of denial trends might reveal areas for staff training and process enhancements. Billing, coding, and clinical staff working together effectively helps to resolve denials quickly and avoid them in the future. Healthcare providers can improve their revenue cycle and make sure they recover as much money as possible by continuing to take a proactive approach to denial management.
10. Leveraging Reporting and Analytics for Insights
Detailed reporting and analysis are critical to optimizing the healthcare revenue cycle. By monitoring KPIs such as aging receivables, denial rates, and clean claim rates, providers gain clear insights into process efficiency and areas needing improvement. Advanced analytics tools uncover trends, optimize workflows, and support data-driven decision-making to enhance financial performance. Predictive analytics further empowers providers to anticipate issues before they escalate, while benchmarking against industry standards highlights best practices and performance gaps.
Regularly reviewing financial and operational metrics ensures the cycle remains agile and effective. These insights not only improve revenue outcomes but also strengthen strategic planning and operational sustainability. With a clear view of performance and proactive measures in place, healthcare organizations can drive efficiency, maintain financial health, and continue delivering high-quality patient care in an increasingly complex environment.
Struggling With Claim Denials? Let Our RCM Experts Optimize Your Billing & Appeal Process Today
How Can RCM Benefit from Agentic AI?
- Proactive Decision-Making: Agentic AI enables real-time, autonomous decision-making in RCM, reducing delays and streamlining processes like claim submission, payment posting, and follow-ups.
- Optimized Revenue Capture: By analyzing large datasets, Agentic AI identifies underpayments, missed charges, and coding errors, ensuring maximum reimbursement and minimizing revenue leakage.
- Enhanced Denial Management: It autonomously detects denial patterns, suggests corrective actions, and initiates timely appeals, improving claim resolution rates and reducing administrative burden on staff.
- Personalized Patient Engagement: Agentic AI tailors financial communications and support based on individual profiles, enhancing patient satisfaction and increasing transparency in billing and payment processes.
Why Choose NextGen Invent?
The future of revenue cycle management is being rapidly transformed by innovative technologies like automation, data analytics, and artificial intelligence. These innovations are accelerating processes, improving accuracy, and minimizing errors, paving the way for more efficient and reliable healthcare financial operations. However, as the RCM process flowchart evolves, it also brings challenges such as navigating ever-changing regulations and ensuring robust data privacy. Meeting these demands requires a proactive, adaptable approach backed by strategic partnerships.
NextGen Invent is a trusted leader in AI healthcare mobile app development services. We deliver end-to-end solutions designed to streamline every phase of the revenue cycle—from accurate coding and billing to swift, compliant claim submissions. Our experienced team customizes each engagement to fit the specific needs of your organization, maximizing revenue, minimizing denials, and boosting operational efficiency.
Partner with us today for personalized, future-ready RCM software services that drive financial and regulatory success.
Frequently Asked Questions About RCM Process Flowchart
Related Blogs
AI in Personalized Medicine: Solving Delayed Diagnoses for Better Patient Outcomes
The rapid growth of new medications, treatment protocols, and evolving regulations is outpacing healthcare providers’ ability to stay updated. AI in personalized medicine helps bridge this gap, enabling timely decisions by analyzing vast data and delivering actionable insights in real-time.
Unlocking Healthcare Innovation through Digital Health Enablement
What defines an effective digital health enablement system? Having quick and easy access to the data you need is undoubtedly important. A few minutes of delay in accessing data could mean the difference between life and death in healthcare delivery organizations where every second matters.
The Crucial Role of Laboratory Management System in Modern Clinical Labs
Does your lab have ongoing difficulties meeting the demands of patient diagnostics? Are out-of-date systems and mistakes made when entering data by hand slowing down your team and affecting patient care?
Stay In the Know
Get Latest updates and industry insights every month.
 1. Optimizing Patient Registration Processes
1. Optimizing Patient Registration Processes