Introducing Provider Revenue Cycle Management – Must-Have RCM Features for Maximum ROI
Implementation failures in RCM often stem from deeper, systemic issues. Sometimes, organizations lack the internal capacity to fully leverage the technology’s potential. Even more concerning, some RCM vendors overpromise as well as underdeliver, leaving providers with disjointed systems and unmet expectations. The real question isn’t if RCM technology works, but why it so often falls short. The answer lies in how strategically it’s chosen, implemented, and aligned with operational goals.

Struggling With Claim Denials? Streamline Approval Rates with Our AI-Driven Revenue Cycle Software Services

“North American AI in revenue cycle management dominated the global market and accounted for the largest revenue share of over 55% in 2024. One of the most significant drivers of artificial intelligence in the revenue cycle management market is the increasing volume and complexity of healthcare claim denials. Claim denials are rising in volume and are increasingly difficult to appeal due to varying payer policies and frequent regulatory shifts. AI-enabled solutions offer predictive denial management, real-time eligibility checks, and automated appeals processing, significantly improving denial resolution rates.”– Grand View Research
Optimizing Financial Operations in Healthcare Through Advanced Revenue Cycle Management Technology
Healthcare organizations today face mounting pressure to streamline financial operations, reduce administrative burdens, and enhance the patient’s payment experience. RCM features have emerged as a critical enabler in addressing these challenges. They offer end-to-end solutions that span from patient registration and insurance eligibility verification to charge capture, coding, billing, claims processing, and final payment collection.
- Modern RCM platforms leverage AI and automation to significantly reduce errors, speed up reimbursement cycles, and improve cash flow.
- Providers now have access to intelligent software for coding accuracy, real-time claims tracking, automated payment posting, and actionable financial reporting.
- Automated kiosks streamline patient check-ins and payments, while electronic payment systems and secure portals offer flexibility and transparency.
- Interactive voice response systems and AI-powered chatbots enhance communication and engagement, minimizing friction and confusion around billing and payments.
Together, these integrated technologies transform the revenue cycle into a strategic asset, driving operational efficiency, accelerating reimbursements, and delivering a more seamless and organized financial experience for both providers and patients.
Importance of Revenue Cycle Management in Healthcare
In the healthcare industry, effective revenue cycle management is critical for a number of reasons. Its primary goal is to ensure that healthcare practitioners are fairly and promptly compensated for their services. Their ability to maintain financial stability allows them to keep providing patients with top-notch care. The payers are shifting from fee-for-service to an outcome or value-based care reimbursement model.
Additionally, RCM features are essential for operational cost optimization. Healthcare organizations can better utilize resources by lowering manual labor, speeding up procedures, and decreasing errors. Consequently, this results in reduced expenses and enhanced overall efficiency.
The Potential of AI in Streamlining Administrative Tasks with RCM Features
Administrative complexity continues to strain healthcare operations, consuming valuable resources, increasing costs, and contributing to staff burnout. In this environment, AI is no longer a futuristic concept; it’s a critical tool for transforming the revenue cycle.
AI presents a powerful opportunity to reduce manual, repetitive tasks that slow down operations and introduce errors. From automating prior authorizations and eligibility checks to optimizing coding accuracy and accelerating claims processing, AI-driven solutions allow healthcare providers to reclaim time, improve accuracy, and focus more on patient care. The strategy is to have AI do many of the mundane tasks, such as patient follow-up, and allow the PFS representatives to do the “critical thinking” work.
By intelligently managing administrative workflows, AI not only improves operational efficiency and cash flow but also enhances the overall patient financial experience.
The Strategic Value of Revenue Cycle Management in Modern Healthcare
Although we will discuss RCM features, the real focus is on how RCM healthcare services affect your daily financial operations and financial results. Here are some practical benefits that can revolutionize your healthcare procedures:
- Minimizes Denials: The foundation of any successful RCM solution is proactive denial management. Driven by integrated coding compliance checks and intelligent denial management tools, it increases revenue capture, minimizes errors from the start, and drastically lowers claim denials.
- Speeds Up the Financial Process: Simple and effective patient billing collection is made possible by your team’s automated follow-up communications and streamlined operations. Lowering administrative workloads and speeding up payments will eventually increase your cash flow and financial stability.
- Boosts Revenue Performance: RCM healthcare services optimize claim submissions, reduce denials, and speed up payments, streamlining the entire revenue cycle. This ensures the practice’s financial stability by translating into a measurable improvement in cash flow.
- Encourages Informed Decision-Making: Making use of real-time data gives you the ability to make wise choices. For long-term financial well-being, RCM features offer insightful information on important indicators that help you spot patterns, streamline processes, and spend resources wisely.
Understanding the Key Stages of Revenue Cycle Management
Depending on the particular organization, the revenue cycle management stages may vary. The revenue cycle in the healthcare sector typically consists of the following phases:
- Pre-Service or Preregistration: Prior to the delivery of the service or product, this phase takes place. It covers elements like pricing prediction, preauthorization for treatments, eligibility, and insurance verification.
- Service or Point of Sale: At this point, the product is sold, or the service is rendered. After that, the company records the transaction and records and codes the charge.
- Billing or Claim Submission: A bill or claim is prepared by the organization and sent to the payer (such as the patient or insurance company) following the service or transaction. Along with claim scrubbing and error repair, this step also entails coding and billing for goods or services.
- Payment Posting & Remittance Processing: Payment is received by the company and credited to the patient’s account when the claim has been processed. Payment reconciliation, appeals, and denial management are all included in this phase.
- Collections: After payment posting, the collections process starts if there are any unpaid amounts. This could entail sending patient statements and bills, working with collection agencies, or setting up payment schedules.
- Reporting & Analytics: During the revenue cycle, the company gathers and examines data to spot patterns, track performance, and enhance procedures. This covers denial and rejection analysis, revenue cycle reporting, monitoring key performance indicators, and efforts to optimize processes.
Tired Of Manual Errors? Automate Billing & Payment Posting with Our AI Healthcare Mobile App Development Services
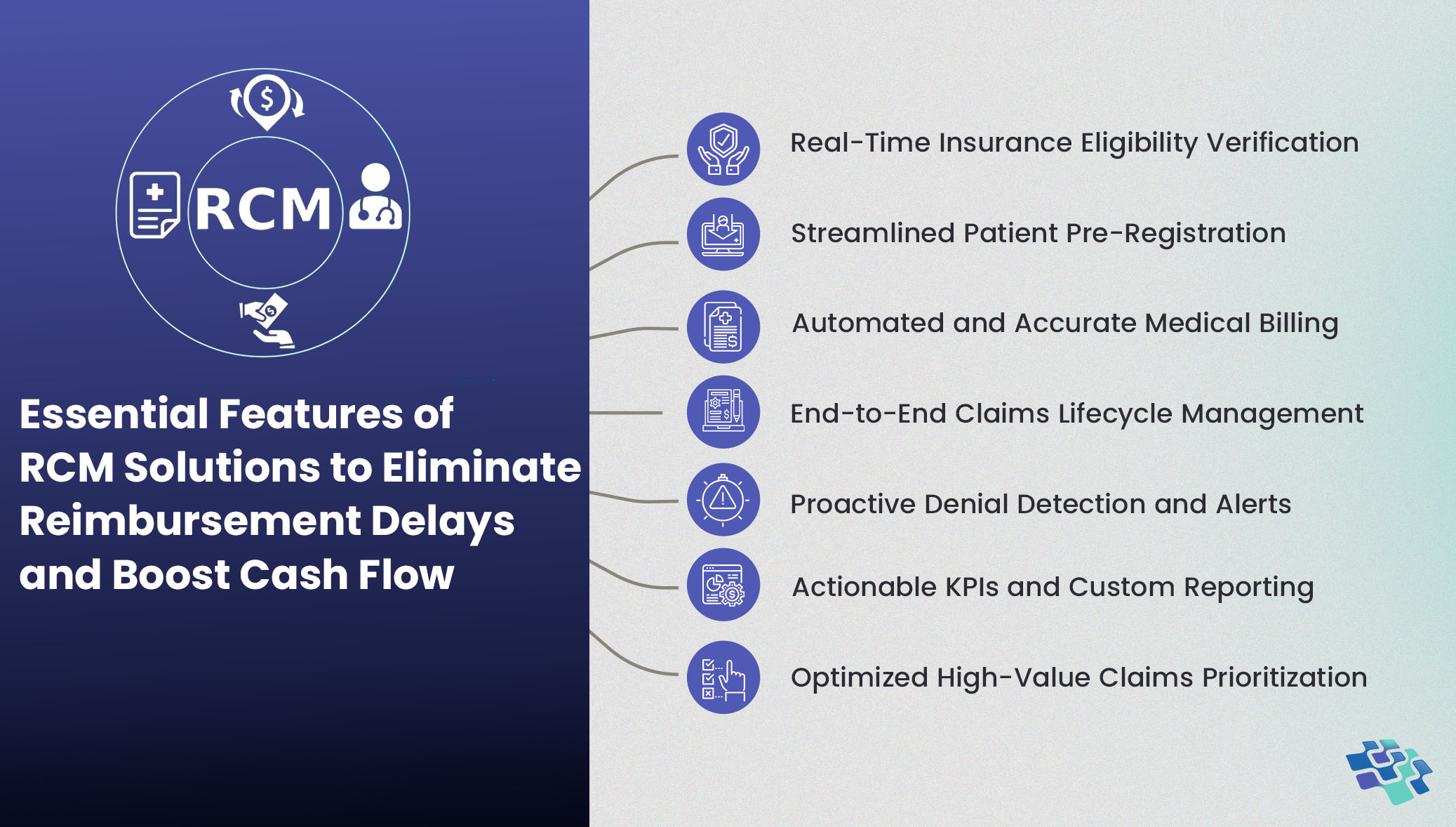
Tackling Claim Denials and Payment Delays: Essential RCM Features Every Solution Must Have
The needs of each healthcare provider determine which RCM features should be included in healthcare. The following list includes some of the most sought-after features of healthcare management systems.
 1. Real-Time Insurance Eligibility Verification
1. Real-Time Insurance Eligibility Verification
By instantly confirming a patient’s coverage details, including co-pays, deductibles, and plan design/benefits, practices can prevent claim denials, reduce reimbursement delays, and ensure financial transparency from the outset. This capability not only eliminates manual verification processes but also empowers front-office staff to make informed decisions at the point of service.
For healthcare organizations focused on operational efficiency and revenue integrity, real-time eligibility checks are instrumental in improving cash flow, minimizing administrative overhead, and enhancing patient satisfaction.
2. Streamlined Patient Pre-Registration
Patient registration typically marks the beginning of a revenue cycle and is one of the most essential RCM processes. However, including the pre-registration option aids in the acquisition and retention of patient data by healthcare providers. Individuals who fall into this category can use healthcare facilities without having to register. When it comes to emergency admissions and emergency healthcare administrations, this process is really helpful.
Future patient records also assist healthcare providers in improving patient engagement, which in turn increases patient loyalty.
3. Automated & Accurate Medical Billing
A healthcare center is where people go to take advantage of countless medical procedures. Their staff cannot possibly recall all of the expenses related to these therapeutic procedures. One way to tackle this difficulty is to incorporate automated billing into the design and implementation of healthcare revenue cycle management services.
To improve the flexibility of payments, include more payment platforms, channels, and alternatives.
4. End-to-End Claims Lifecycle Management
Increase the precision of the submitted claims by automating the procedure. This procedure can be made clear by revenue cycle management for custom AI healthcare mobile app development services, which notify patients in advance of their insurance qualifying requirements. Patients will therefore be better equipped and have more control over their course of treatment.
The requirements for filing and accepting or rejecting claims vary depending on the insurance company. It is possible to create automated RCM features that can submit personalized claims according to the requirements of each insurance company. Both claim rejection and claim filing time will decrease as a result.
5. Proactive Denial Detection & Alerts
The use of denial alerts is another crucial component of future RCM solutions. Using the RCM platform’s automatic feature that predicts denial probabilities is the simplest method to reduce denials. These RCM features allow any member of the medical billing team to swiftly remedy the issue through re-coding, flagging denied claims.
Healthcare interoperability and provider revenue cycle management systems boost employee productivity. They also provide a smooth payment processing flow throughout the company.
6. Actionable KPIs & Custom Reporting
An evaluation of the organization’s general health is a review of the revenue cycle management system. Consequently, when KPIs and periodic reports are easily accessible for staff meetings and other uses, they can be quite helpful. The practice’s financial health can be significantly improved by using revenue cycle management software that can give these reports automatically and regularly.
For further benefit, these reports can also include other elements, such as population health management and Social Determinants of Health data. Financial reports, insurance procedures, an examination of timely completion of billing-related tasks, and pertinent paperwork can all be included in weekly reports and KPIs.
7. Optimized High-Value Claims Prioritization
Every healthcare organization wants to use healthcare automation to retain high profitability. Making sure that claims are submitted using medical informatics to their fullest potential is crucial to reaching this objective. Healthcare providers can achieve success with revenue cycle management by adhering to the highest value submission standards. Since the claim value is at its maximum when this policy is integrated into the RCM program, it can offset the impact of possible reimbursement reductions.
Errors can be prevented, and claims values can be better tracked with a hospital-based physicians’ RCM solution that is well-integrated. The healthcare facility can anticipate a higher bottom line; claims are processed more quickly through electronic data sharing, and there is less manual intervention.
Losing Revenue to Inefficient Workflows? Optimize Operations with Our Custom-Built AI Healthcare Software Solutions
Potential Risks & Challenges of Implementing AI in Revenue Cycle Management
- Data Quality & Accuracy: Data is crucial to the training and decision-making processes of AI algorithms. Improper, biased, or insufficient data can result in improper billing, poor forecasts, and possible financial losses. Maintaining accuracy requires constant monitoring, appropriate data preprocessing, and data integrity.
- Lack of Explainability: Deep learning neural networks and other AI models are frequently referred to as “black boxes” due to the difficulty in explaining how they make decisions. Concerns over the methods used by AI algorithms to reach conclusions or forecasts may arise from this lack of openness. Achieving a balance between precision and the capacity to clearly explain AI system judgments is crucial in the context of RCM.
- Resistance to Adoption: Employee resistance to AI implementation in RCM may stem from concerns that AI technology will replace them or change current workflows. To achieve adoption and optimize the advantages of AI in RCM, it is imperative to overcome opposition and make sure that appropriate training and change management initiatives are in place.
- Regulatory Compliance: The healthcare sector is highly regulated, with laws and rules controlling insurance reimbursement, billing procedures, and patient data protection (including HIPAA in the US). These regulations, which can be complicated and prone to change, must be followed by AI systems. Avoiding legal and financial repercussions requires that AI models and procedures adhere to all relevant laws and regulations.
Conclusion
Investing in comprehensive RCM healthcare services is no longer optional. Healthcare providers need to enhance financial performance, reduce administrative burden, and deliver superior patient experience. Core capabilities such as efficient claims management, automated payment posting, real-time eligibility verification, advanced reporting, and strong compliance safeguards are critical for streamlining workflows and accelerating revenue collection.
NextGen Invent’s AI healthcare mobile app development services take this a step further by enabling seamless integration of RCM features. This empowers staff and patients with real-time access to eligibility checks, billing information, and payment options, anytime, anywhere. With intelligent automation and user-centric design, our RCM healthcare services help providers improve cash flow, optimize operational efficiency, and support better care delivery at every stage of the revenue cycle.
Frequently Asked Questions About RCM Features
Related Blogs

The RCM Process Flowchart That Solves Claim Denials & Payment Delays
Revenue cycle management systems streamline billing by centralizing financial processes for greater efficiency and accuracy. With growing complexity in care, isn’t it time your organization considered a smarter approach to billing?
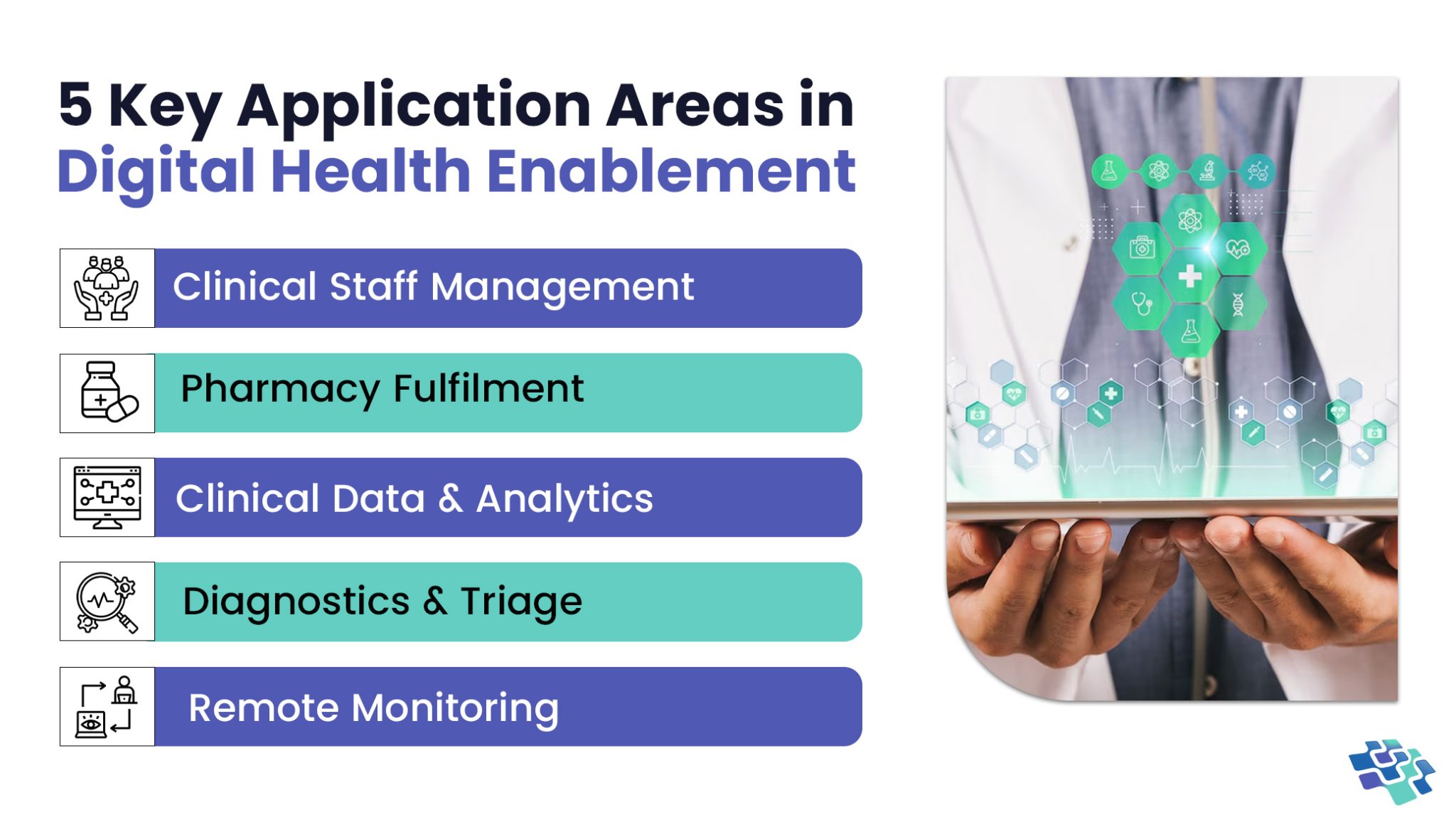
Unlocking Healthcare Innovation through Digital Health Enablement
What defines an effective digital health enablement system? Having quick and easy access to the data you need is undoubtedly important. A few minutes of delay in accessing data could mean the difference between life and death in healthcare delivery organizations where every second matters.
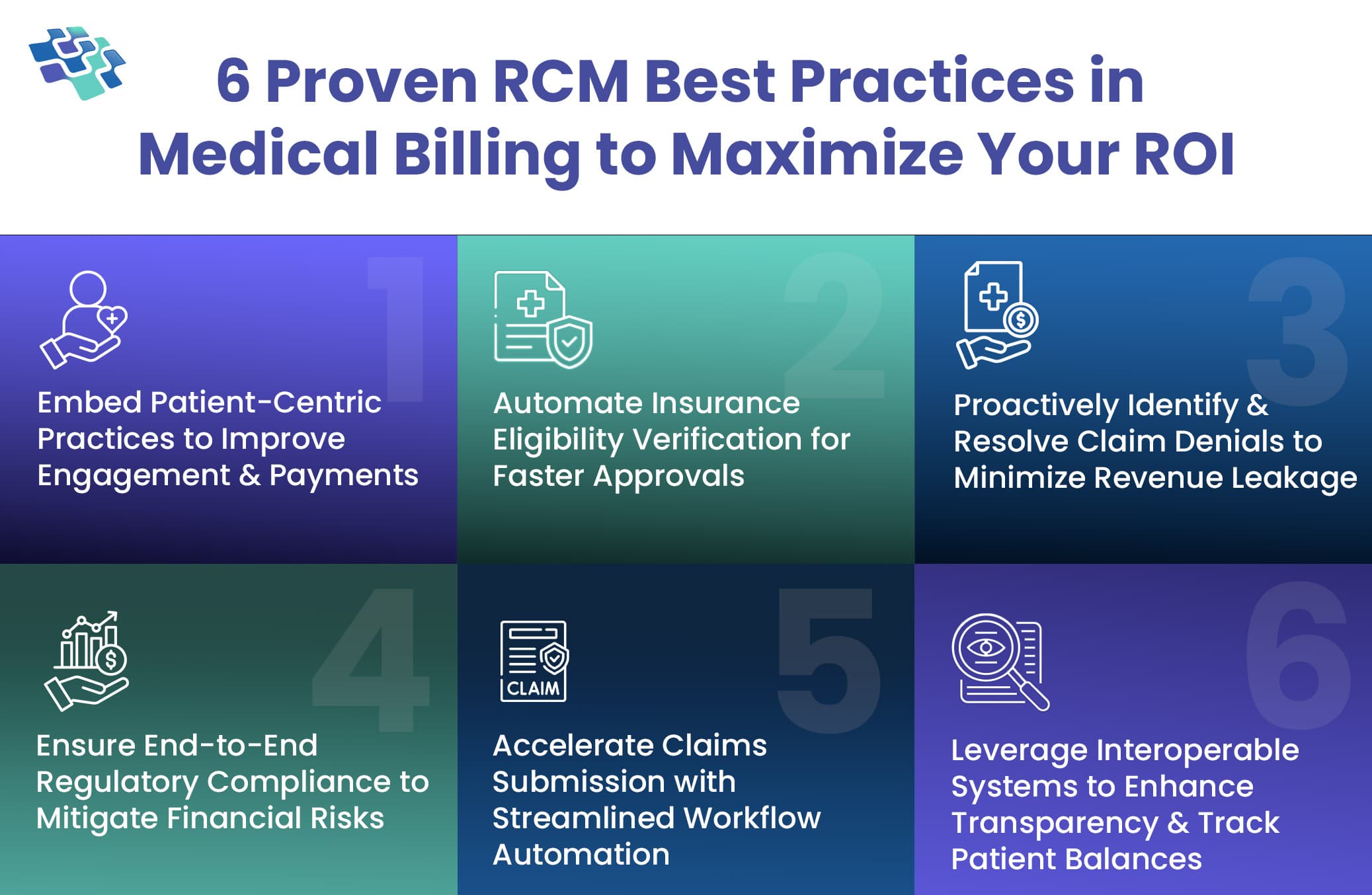
RCM in Medical Billing: Fix Denials, Delays, and Disruptions with These 6 Proven Best Practices
Revenue cycle management is a crucial process in healthcare that governs the financial operations, ensuring providers are accurately compensated for their services. But have you ever wondered what truly keeps the financial engine of a healthcare organization running smoothly?
Stay In the Know
Get Latest updates and industry insights every month.
 1. Real-Time Insurance Eligibility Verification
1. Real-Time Insurance Eligibility Verification